"Virtual Surgery" shows surgeons how wounds will heal
“My field of expertise is soft tissue biomechanics,” said Adrian Buganza, assistant professor of mechanical engineering at Purdue. “Specifically, I’m interested in how skin deforms and adapts to physical forces, and how this affects skin growth and wound healing. And this is particularly important when it comes to reconstructive surgery.”
Buganza discovered that surgeons largely function by intuition and “feel” when assessing the skin of a patient. “They have an inherent understanding of the mechanics,” said Buganza. “They know that stretching the skin in certain places will likely introduce complications in the healing process. But I was surprised to learn that there are no tools available to them to measure this tension, and give them quantifiable options.”
Buganza and his team created a new methodology to predict how skin will heal, and verified the process in a real-world surgical case. They published their results in the Journal of Biomechanics.
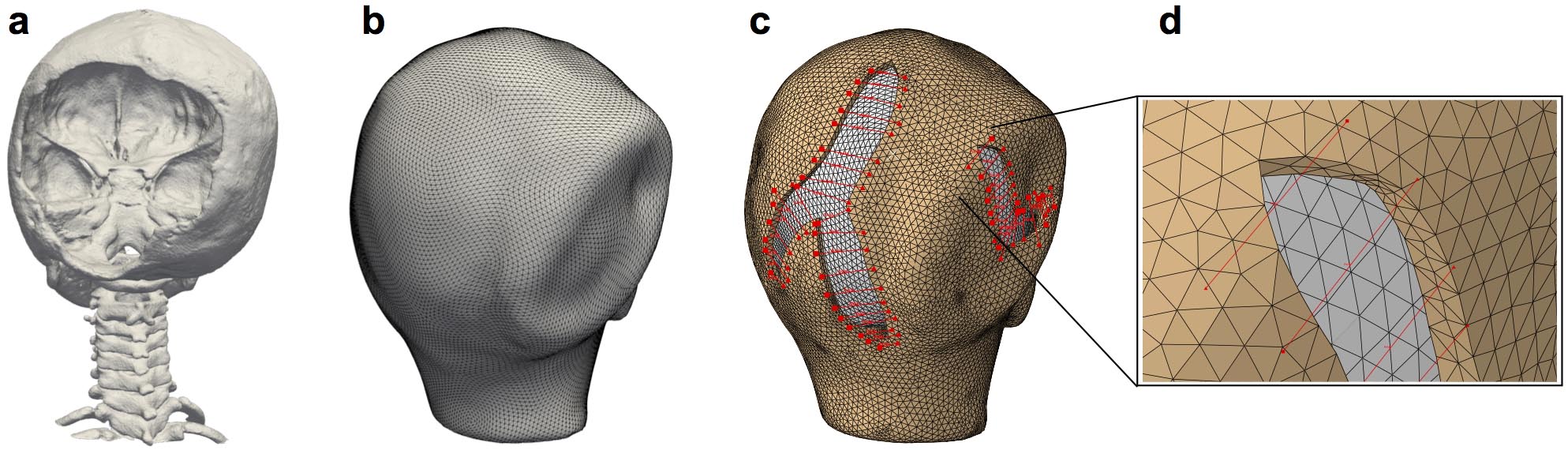
Step one involves creating a 3D geometry of the affected area. While there are specialized cameras that can create 3D images, Buganza discovered that taking smartphone photos from different angles, and stitching them together using off-the-shelf computer software, creates a sufficiently accurate model. Step two involves testing the elasticity of the skin, using a small suction device. “Once the computer has those two elements -- the geometry and the skin’s mechanical properties -- then we can build the computer simulation using finite element analysis,” said Buganza.
Before the surgeon ever makes an incision, the software can perform “virtual surgery” -- showing the most likely outcome of the healing process, and indicating where complications are likely to occur. Based on the data, the surgeon may choose to cut in a different way, in order to minimize the potential healing problems.
“We’ve been using these kinds of engineering tools for analyzing buildings of concrete and steel,” said Buganza. “And skin is no different. It’s a material. It may be more complex, but at the end of the day, skin does obey the laws of physics!”
“The best part about virtual surgery is that we can do it many times,” said Buganza. “It’s not just one shot. We can give the surgeon many different options, and offer statistical probabilities of which option will be best for the patient. This kind of personalized medicine -- using computational models to predict tissue behavior of each patient -- has the potential to completely change the way these procedures are performed.”
Writer: Jared Pike, jaredpike@purdue.edu
Source: Adrian Buganza, abuganza@purdue.edu
Adrian Buganza's lab: https://engineering.purdue.edu/tepolelab
Multi-view stereo in the operating room allows prediction of healing complications in a patient-specific model of reconstructive surgery
Taeksang Lee, Sergey Y. Turin, Arun K. Gosain, Adrian Buganza Tepole
https://doi.org/10.1016/j.jbiomech.2018.04.004
Abstract
Excessive mechanical stress leads to wound healing complications following reconstructive surgery. However, this knowledge is not easily applicable in clinical scenarios due to the difficulty in measuring stress contours during complex tissue rearrangement procedures. Computational tools have been proposed as an alternative to address this need, but obtaining patient specific geometries with an affordable and flexible setup has remained a challenge. Here we present a methodology to determine the stress contours from a reconstructive procedure on a patient-specific finite element model based on multi-view stereo (MVS). MVS is a noninvasive technology that allows reconstruction of 3D geometries using a standard digital camera, making it ideal for the operating room. Finite element analysis can then be used on the patient-specific geometry to perform a virtual surgery and predict regions at risk of complications. We applied our approach to the case of a 7-year-old patient who was treated to correct a cranial contour deformity and resect two large areas of scalp scarring. The simulation showed several zones of high stress, particularly near the suture lines at the distal ends of the flaps. The patient did show delayed healing and partial flap tip necrosis at one of such predicted regions at the 30-day follow up visit. Our results further establish the application of computational tools in individualized medical scenarios to advance preoperative planning and anticipate regions of concern immediately after surgery.
