Bumsoo Han receives $4.7 million to fight pancreatic cancer
"Pancreatic cancer poses significant healthcare, economic, and societal challenges," said Han, professor of mechanical engineering. "This research will test a promising new idea of targeting the blood clotting system to improve drug delivery and efficacy for treating this disease."
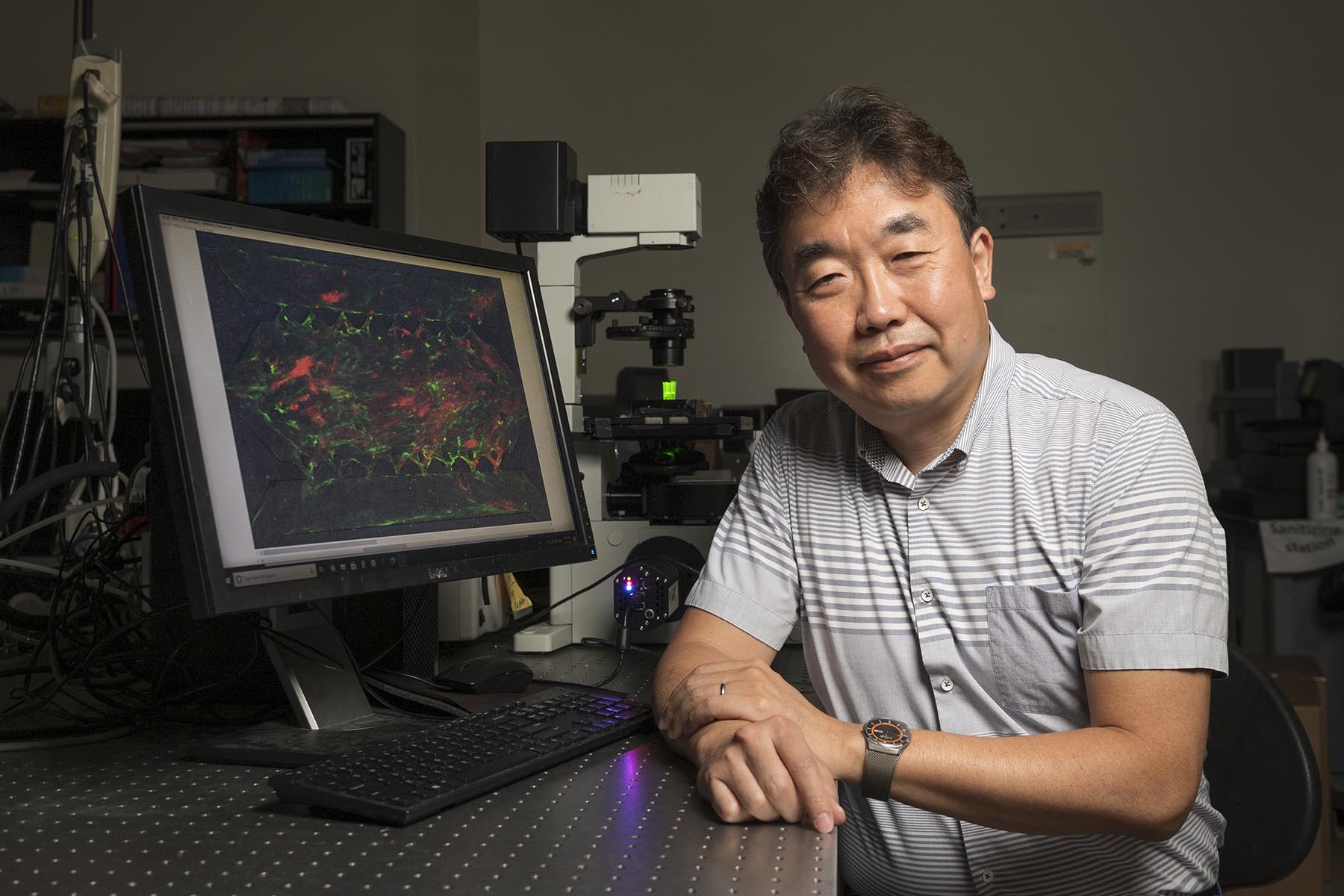
For years, Han has been building tumor microenvironments (TME) on microfluidic platforms, in which he can test therapies on cancerous cells in a laboratory setting to determine which treatments might be applicable to patients. What normally takes 10-to-20 years to develop in a human body, his models can reproduce in just two weeks. He has even used these tools as a "time machine," reversing the growth of cancerous cells and converting them back to their normal state.
This grant is part of a National Cancer Institute program called the Pancreatic Ductal Adenocarcinoma Stromal Reprogramming Consortium (PSRC). The grant is for $4.7 million over five years, with Han as the principal investigator. Other collaborators include co-investigator Dr. Timothy Ratliff, Distinguished Professor of Comparative Pathobiology at Purdue; Dr. Matthew Flick from University of North Carolina; and Dr. Melissa Fishel from Indiana University School of Medicine.
"We look forward to developing this research to investigate ways to genetically reprogram these cancerous cells," said Han. "Hopefully we can play a role in developing new therapies to combat this lethal disease."
This work is supported by the Purdue Institute of Drug Discovery at Discovery Park; and the Purdue Center for Cancer Research, which is one of only seven National Cancer Institute Basic Laboratory Cancer Centers in the nation.
Source: Bumsoo Han, bumsoo@purdue.edu
Writer: Jared Pike, jaredpike@purdue.edu, 765-496-0374
PROJECT SUMMARY
The overarching goal of this research program is to identify therapeutic strategies to convert the stroma of pancreatic ductal adenocarcinoma (PDAC) to a chemo- and immune-sensitive tumor microenvironment (TME). PDAC is characterized by a desmoplastic stroma that facilitates tumor growth/invasion, chemoresistance of pancreatic cancer cells (PCC), and immunosuppressive TME. Highly packed cancer-associated fibroblasts (CAFs) and dense extracellular matrix (ECM) are hallmarks of the PDAC stroma and constitute physical drug delivery barriers. Several stromal components have been targeted to enhance drug delivery, but recent studies have suggested anti-tumor roles for the stroma as complete ablation of stromal components leads to more aggressive tumors. New strategies are highly desired to reprogram stroma without compromising its anti-tumor roles. The central hypothesis is that the coagulation system in the PDAC TME can be targeted to reprogram PDAC stroma to overcome chemoresistance, drug delivery barriers, and immunosuppressive TME. Cancer- associated coagulation has been reported as a key functional signaling pathway in PDAC. Notably, several coagulation molecular targets, including thrombin, protease-activated receptor 1 (PAR1), and fibrinogen/fibrin, have been implicated in important roles contributing to tumor progression and therapeutic resistance. Specifically, it is hypothesized that the thrombin-PAR1 signaling axis can be targeted to suppress PCC growth/invasion and CAF growth/fibrosis. In addition, thrombin-mediated fibrin deposition can be targeted to suppress the drug delivery barrier and immunosuppressive TAM activities, which suppresses anti-tumor T cell activities. This hypothesis will be tested mechanistically and evaluated for translational potential by pursuing the following two integrated aims: Aim 1) Mechanistic Research: Determine the contribution of the coagulation targets in the PDAC TME. Specifically, the team will determine the role of thrombin-PAR1 signaling axis to CAF-mediated fibrosis, thrombin-mediated fibrin deposition on drug resistance, and PAR1/fibrin on the immunosuppressive TME. Aim 2) Translational Research: Evaluate the pharmacological inhibition of the coagulation targets. Especially, the team will expand the mechanistic understanding from Aim 1 using patient- derived PDAC models with FDA-approved inhibitors of thrombin and PAR1, and fibrinogen depleting agents. The effects of pharmacological inhibition will feedback to Aim 1 to delineate the efficacy of inhibiting coagulation targets. The outcome of this research will establish a new mechanistic understanding of the role of coagulation activities in the PDAC TME. It will determine whether blockade of the coagulation is a promising strategy to reprogram the PDAC stroma and, ultimately, suppress PCC/CAF growth and improve drug delivery and efficacy.
