2022 Senior Design Projects
-
Low-Cost 3D-Printed Ventilator Splitter
-
The WatchDog: A Blood Transfusion Equipment Accessory for Efficiency and Safety
-
Reusable Cooling Pack for Solid Organ Transport
-
Simultaneous Breastfeeding for Babies with Cleft Palate
-
Piezoelectric Material Integration for Doppler Ultrasound Assisted Catheter Placement to Improve Treatment Visualization in Interstitial Brachytherapy
-
Endovascular Intervention For Pulmonary Hypertension in Newborns
-
Objective, Non-Invasive Method for Monitoring Hydrocephalus in High-Risk Infants
-
Smartphone application to help the blind in use of public transportation services in Montevideo, Uruguay
-
Low Cost MRI Compatible Olfactometer
-
Low-cost Biomarker Monitoring for Chronic Pediatric Asthma in the U.S.
-
EpicPen: A Reusable, Replaceable Epinephrine Auto-Injector
-
Pepsin Fluidics: An Innovative Laryngopharyngeal Reflux Diagnostic Device for Accuracy and Patient Comfort
-
A low-cost mechanical prosthesis knee design to improve accessibility in low-income populations
-
Near-infrared (NIR) imaging used to detect nerve health
-
Design and Feasibility of Novel Peritoneal Dialysis Catheter to Prevent Mechanical Dysfunction in Neonate Patients
-
Atraumatic Cervical Clamp to Reduce Pain & Bleeding Associated with IUD Insertion Procedure
-
iOS Application for Visually Impaired (Total or Partial) Diabetic Patients that provides Audio Readouts of Glucometer Readings
-
The Fiberoptic Bronchoscopy System for Detection of Aspiration Severity
-
InManage - Inpatient Rehabilitation Management System
-
Electromyographic Classification of Tetanus in Low Resource Settings
-
Mucus Protein Biomarker Detection for Diagnosis of Chronic Rhinosinusitis
-
An Automated Method for Classifying Unhealthy vs Healthy Nerve Tissue in Open-Surgery Applications
-
Temperature Controlled Blood Transport Container Using Thermoelectric Cooling
-
Low-Cost Upper Limb Prosthetic for Tanzania
Low-Cost 3D-Printed Ventilator Splitter
Sam Irons, Hannah Hill, Greyson Moroney, Lindy Parr, Zeke Huls

In 2019, there were an estimated 60 ventilators supporting the 63.5 million citizens of The United Republic of Tanzania. While the COVID-19 pandemic exacerbated the major weakness in the ventilator inventory of developing countries, there are an abundance of other illnesses that often require mechanical ventilation. Patients suffering from strokes, pneumonia, collapsed lungs, sepsis and many other conditions frequently require mechanical ventilation. Ventilator splitting as a solution for increasing the patient capacity of available ventilators has been used before, but it has lacked many critical features necessary for design success. To be successfully implemented, the developed ventilator splitter must eliminate the concern of cross contamination between two patients, allow for flow control between the patients, maintain each patient’s blood oxygen levels at 95% or higher, and meet patient specific tidal volumes with at least 95% accuracy. In order for the solution to be innovative and able to be utilized in developing countries, it must cost significantly less than purchasing an additional ventilator.
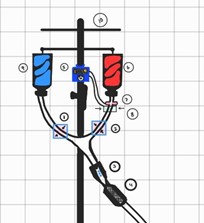
The WatchDog: A Blood Transfusion Equipment Accessory for Efficiency and Safety
Sumantika Sekar, Erika Huber, Mei Phillips, Aikya Chirra, Youssef Beshay
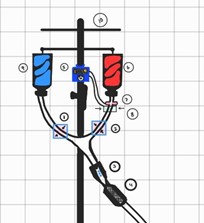
Blood transfusion is a common and critical procedure, as 14 million units of blood are transfused yearly in the US. A key step in the transfusion process is the switchover near the end of transfusion from the empty blood bag to saline. This is a relatively easy step but it is critical to avoid trapping air in the tubing, which could cause a fatal air embolism in the patient. Unfortunately, inaccurately labeled blood bags create an unpredictable error in the process of transfusion when nurses program the pump rate and time. Consequently, nurses are required to frequently monitor the patient and either reprogram the pump or end the process early and dispose of the transfusion tubing containing the remaining blood product when air is present at the end of transfusion. There is a need to rapidly detect any large air bubble within blood transfusion tubing near the end of transfusion and to automatically halt the procedure if a large air bubble is detected. A solution for this need will decrease the risk of air embolism, improve resource management, and increase nurse availability for patient care. The team presents a low-cost, compact device called the WatchDog, which attaches to the transfusion tubing to monitor the line for air directly below where the blood bag is connected to the tubing. This device will also occlude the tubing upon detecting a continuous segment of air. The main components of this reusable device include the air bubble sensor and occlusion system connected by a microcontroller and motor. The WatchDog innovatively leverages the pre-existing feature of blood transfusion pumps to detect an up-stream occlusion and stop transfusion using a clamping mechanism. The launch of this product would, on average, prevent the waste of 30 milliliters of blood that occurs when a single tubing set is thrown away. Additionally, it will allow nurses to comfortably over-program blood pump rates with minimal patient monitoring so they can dedicate more time to other patient care. Overall, this device can prevent harm and save precious resources in the health care setting.
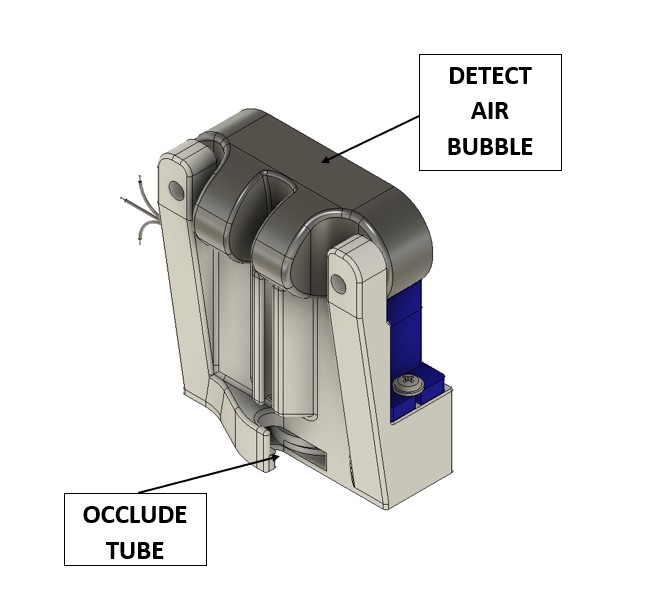
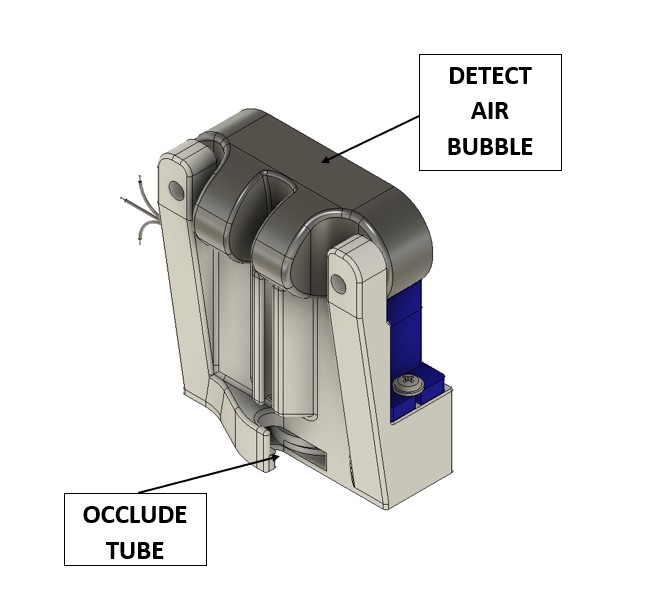
Reusable Cooling Pack for Solid Organ Transport
Crosley Stanley, Emily Lothamer, Tucker Ross, Michael Sullivan, Ryan Hurst
Lung transplants have only a 50% survival rate after 5 years. The most common cause of complications arises from Primary Graft Dysfunction (PGD), a condition in which the lungs spontaneously and rapidly fill with fluid for no known reason. One hypothesized contributing factor of PGD is improper cooling temperature of lungs during transport. The current industry standard is to use ice as a cooling solution, however ice cools the donor lungs below their ideal temperature (to the 0 - 4℃ range), contributing to incidents of PGD. Studies show cooling lungs between 7 - 10℃ results in increased lung viability post transport and decreased chance of developing PGD. PARAGONIX’s LungGuard is the only currently available market solution that is able to maintain the lungs for 12 hours within the desired 7 - 10℃ window. However, the LungGuard is non-reusable and costs $10,000 per use. There is, thus, a need for a solution that will maintain the donor lungs in the more optimal temperature range of 7 - 10℃ for 12 hours while being reusable and low cost. Our product, the OPTIML (Organ Procurement Transportation Isothermal Management for Lungs) Pack, is a zippered,vinyl, cylindrical shell that fits over the lungs, containing silicone “ice” cubes full of acetic acid-water solution (Figure 1). The OPTIML pack takes advantage of the thermochemical property where substances retain a given temperature for prolonged periods of time during phase change. Our cooling pack contains an acetic acid-water solution with a calculated freezing point just over 8°C and a specific heat high enough to slow heat transfer for the desired 12 hour time window. The cooling pack is reusable and can be stored in a conventional kitchen freezer (typically 0°C) prior to use. The silicone cubes help diffuse and prolong the cooling effect and can be individually replaced as they wear out. When scaled, it is predicted that the OPTIML Pack will address the needs of the lung transport process by staying in the range of 8-10°C for 12 hours, as well as by being reusable and costing $172. This solution should enable hospitals to invest in a multiple-use solution that improves the outcomes of lung transport without adding to the $73,000 that it currently costs to procure a lung. In the future, a similar thermochemically-based strategy may be used to cool other organs at more ideal temperatures (hearts, liver, kidney, etc).
Simultaneous Breastfeeding for Babies with Cleft Palate
Ari Atlas, Madeline Kiss, Kayla McKeague, Kaitlyn Murphy, and Olivia Osuch

The act of breastfeeding promotes emotional bonding and allows for direct feeding of breast milk which is the gold standard source of nutrition for infants because it digests easier than formula, provides immune system enhancement and protection for the infant, and contributes health benefits to the mother. Approximately 1 in every 1,700 babies is born with a cleft palate, an opening in the roof of the mouth, preventing them from producing the suction necessary to expel breast milk to directly breastfeed. Because of this challenge with breastfeeding, emotional bonding between the baby and the mother is reduced, and these babies may not receive the full benefits of breast milk as mothers may resort to formula feeding due to the time-consuming process of pumping then bottle feeding. Therefore, there is a need for a method of feeding infants with a cleft palate that provides the nutritional and immune benefits of breastmilk, is time efficient, and facilitates close contact between baby and mother. Our proposed solution incorporates innovative aspects to address the physiological problem by integrating a palate obturator that occludes the cleft with an external guard based off of common pacifier designs, allowing the baby to generate suction needed to feed while protecting from choking hazards. As the only device on the market that offers a new method of direct feeding of breast milk for babies with cleft palates, we reduce the time required and the emotional stress on the mothers.
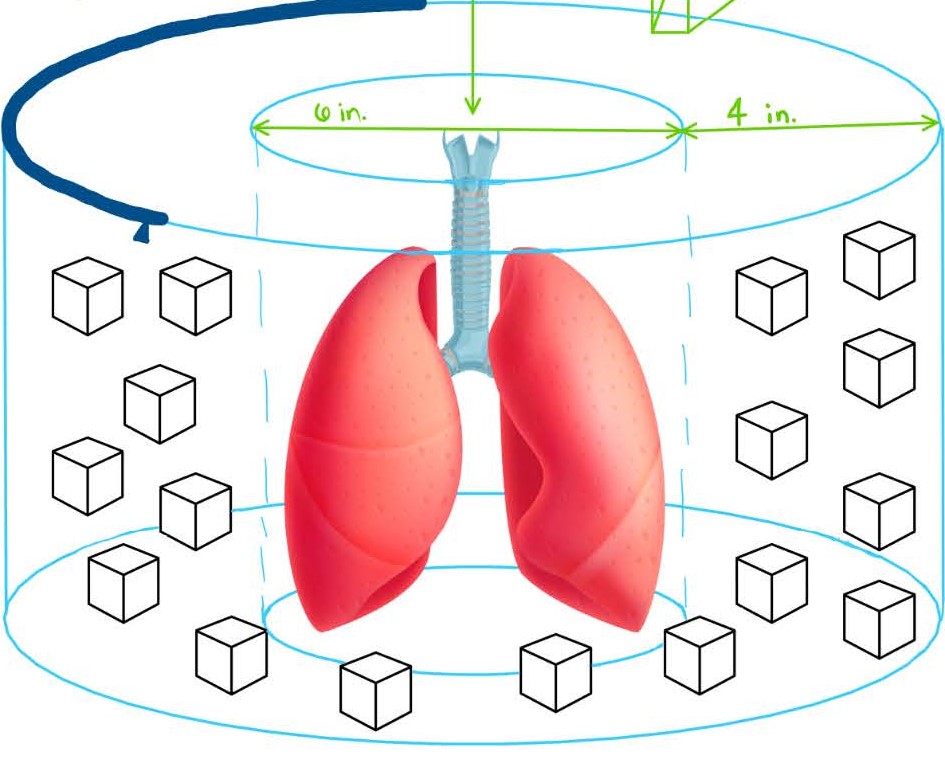
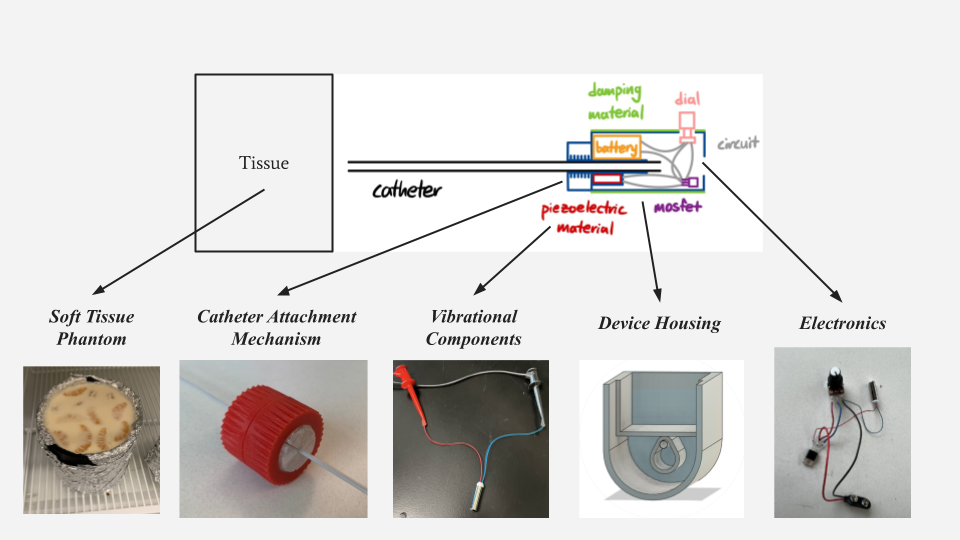
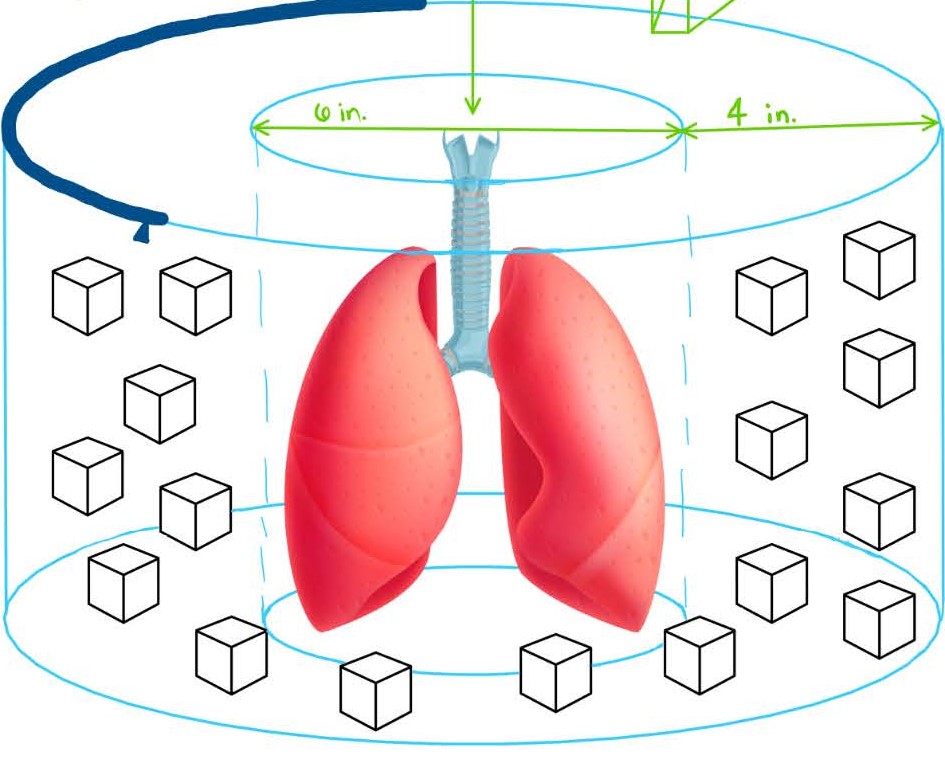
Piezoelectric Material Integration for Doppler Ultrasound Assisted Catheter Placement to Improve Treatment Visualization in Interstitial Brachytherapy
David Kim, June Kim, Marina Murphy, Natalie Romick, Jadah Eshenaur
Interstitial brachytherapy is a therapeutic method for prostate, uterine, cervical, and other soft-tissue cancers which utilizes catheters to deliver high doses of radiation directly to target tissues. To ensure proper internal guidance to the tissue of interest, the catheters are placed under direct ultrasound (US) guidance in the operating room, with post-operative position confirmation with computer tomography (CT) scan. Due to the highly localized nature of the treatment, the placement of brachytherapy catheters using transabdominal/transrectal US in the operating room is vital to the treatment’s effectiveness and patient outcome. However, operational variations and limitations to US can incite poor catheter visualization, which can lead to ineffective treatment, excessive radiation to non-target tissues, or catheter intrusion into surrounding organs. Therefore, there is a need for a device or method to improve the visualization of brachytherapy catheters for radiation oncologists in an operating room setting to improve patient and professional satisfaction, as well as to optimize the accuracy of catheter placement. To address this need, our team has designed a piezo material-integrated catheter attachment which upon electrical input, creates mechanical vibrations that can be detected and visualized using Doppler US. This low-cost, 3D-printed design involves zero contact with the patient, making it easily integrable into established interstitial brachytherapy workflows while offering highly specific control over the location and magnitude of Doppler visualization with catheter detachability and dial-regulated voltage/vibration adjustment. In providing this improved visualization, our device will provide a palpable impact on
medicine through an increase in catheter visualization not only in interstitial brachytherapy, but also other ultrasound-guided procedures with limited visualization.
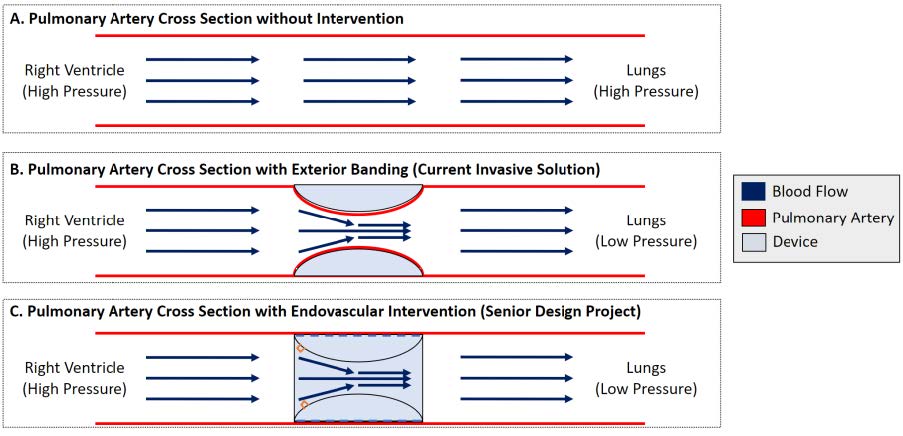
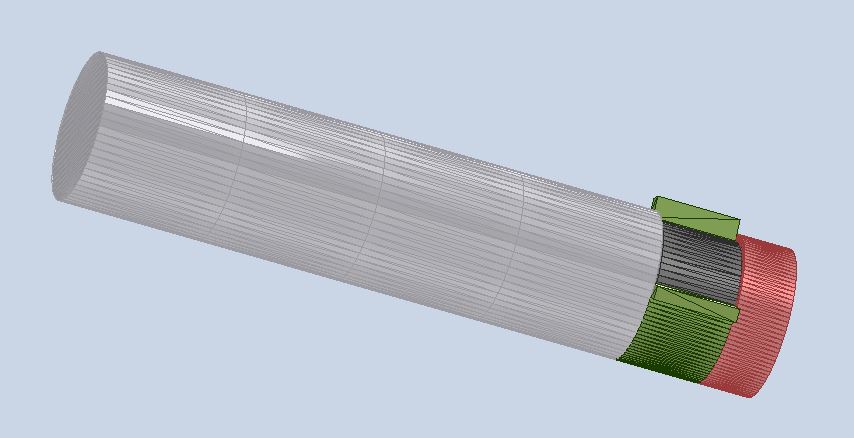
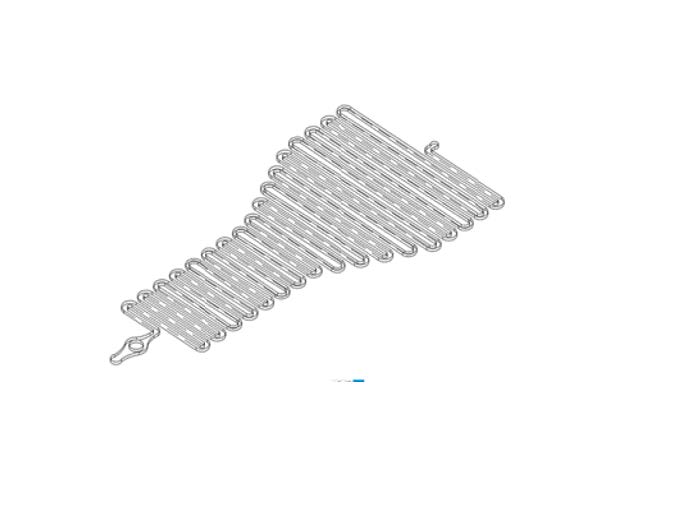
Endovascular Intervention For Pulmonary Hypertension in Newborns
Sam Zhang, Karthik Annamalai, Shivani Pulugura, Scott Malloy, Andrew Darling
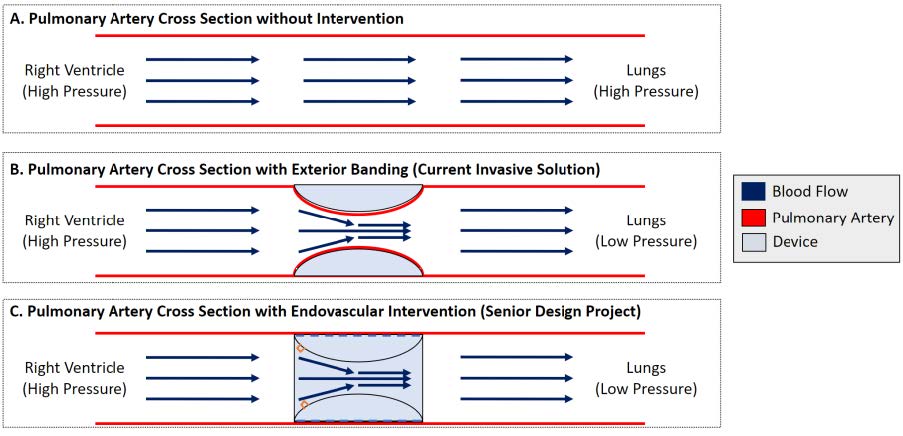
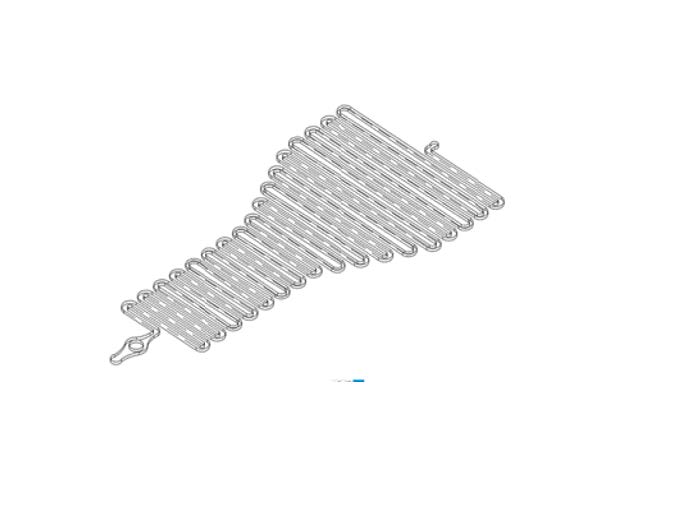
There are about 16,800 births annually in the US that have ventricular septal defects (VSD), in which there is a hole in the wall separating the ventricles of the heart. Newborns requiring intervention are implanted with a device known as a VSD occluder. This device closes the holes to restore normal function, however implantation is delayed for 6-12 months for the newborn to develop and reduce complications. For this time, the newborn is subject to pulmonary hypertension (PH) because of the VSD (A), so a pulmonary artery band is placed through an incision between the babies’ ribs, known as a thoracotomy, to narrow the PA from the outside and reduce pulmonary pressure (B). Removal involves another thoracotomy, which has long recovery and higher risks compared to other minimally invasive procedures. Therefore, there is a need for a minimally invasive device to manage PH in newborns with VSDs to reduce the burden of open surgeries. To address the clinical need, we will create a stent-based occlusion device that restricts flow in the PA. A catheter is placed in the femoral artery and navigated to the PA where a balloon catheter will inflate the device into the vessel wall. The device would occlude blood flow, reducing PH and associated risks (C) for up to 12 months, until the VSD can be repaired. Lastly, the device will have bars for a retrieval device to hook onto, to recompress the device, and remove it through a catheter without causing any damage to the vessel wall. The solution presents itself within a market gap for minimally invasive solutions to this clinical need. To differentiate from current solutions, a large emphasis is placed on the catheter deployment as well as retrieval after 6-12 months. Ultimately, the goal of this solution is to reduce the overall burden on the patients, meaning retrieval will be minimally invasive as well reducing risk to the patient. The solution will utilize a bioresorbable exterior that is left behind when the device is recompressed, in order to avoid damaging the wall. This will continue to support the pulmonary artery until it degrades over a controlled period.
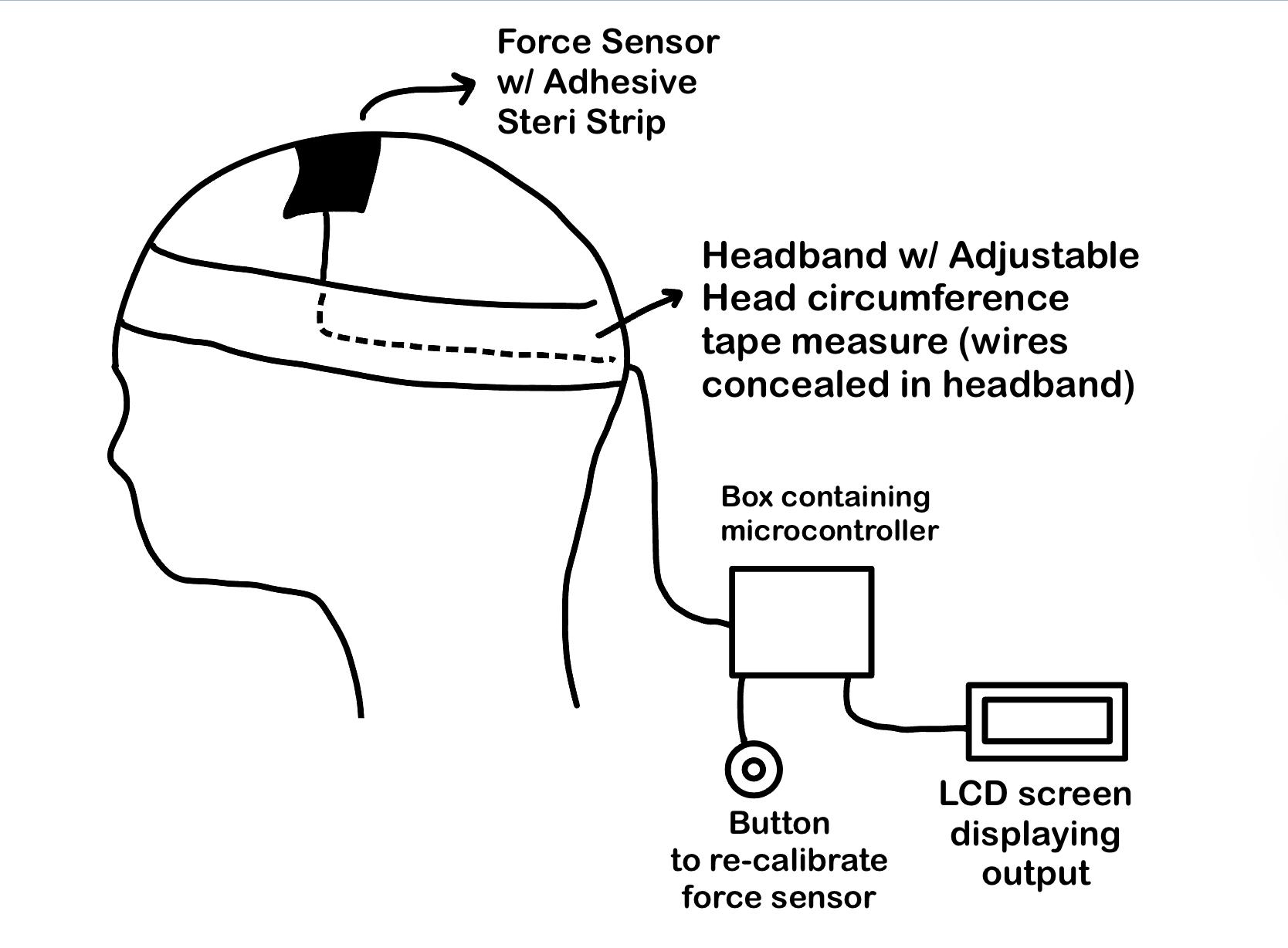
Objective, Non-Invasive Method for Monitoring Hydrocephalus in High-Risk Infants
Emily Bultinck, Tori Litz, Kiernan Schuerman, Harold Paul Pey Tan, Lauren Wimsatt
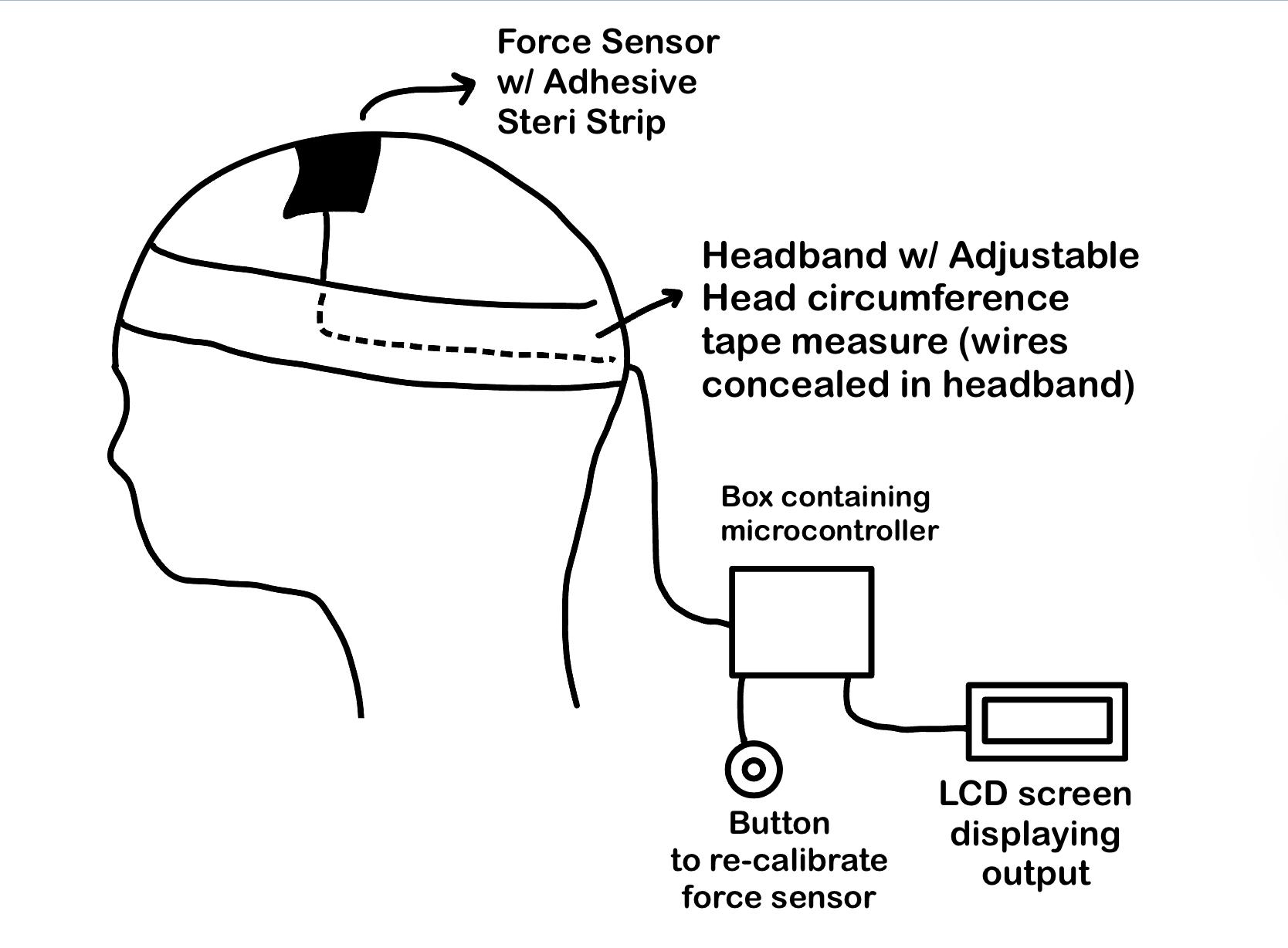
Pediatric hydrocephalus is an abnormal buildup of cerebrospinal fluid in the ventricles of an infant’s brain, leading to increased intracranial pressure (ICP) that can cause brain injury or death if untreated. Complications associated with current ICP monitoring in infants, ages 0-1 years old, at risk of developing hydrocephalus, leads to inaccurate measurements, additional healthcare cost, and additional medical interventions. Therefore, there is a need for an improved method to detect increased ICP in infants at risk of developing hydrocephalus that provides objective, sensitive, and reproducible ICP measurements. Our proposed solution includes a force sensor integrated into a wearable interface that will monitor changes in anterior fontanelle pressure and overall head circumference over time; this solution will provide physicians with a repeatable measurement to increase quality of care and confidence of diagnosis. The pressure sensor is located on top of the head, as shown in the image, and is able to measure the change in geometry of the anterior fontanelle. The output is displayed on an LCD screen, with a microcontroller converting analog data to digital. The configuration of the different components is illustrated in the figure above. This solution is innovative in several ways, as it is noninvasive, easy to implement into current workflows, and requires no machine learning or complex algorithms present in current practices. Overall, this solution will lead to a reduction in cost, risks and probability of inaccurate measurements during ICP measurement procedures.
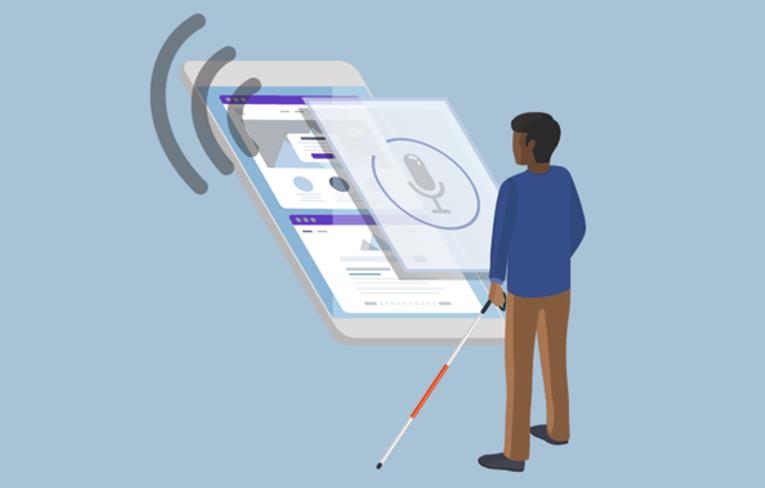
Smartphone application to help the blind in use of public transportation services in Montevideo, Uruguay
Noor Gulrajani, Jonah Adler, Anirudh Sivarajan
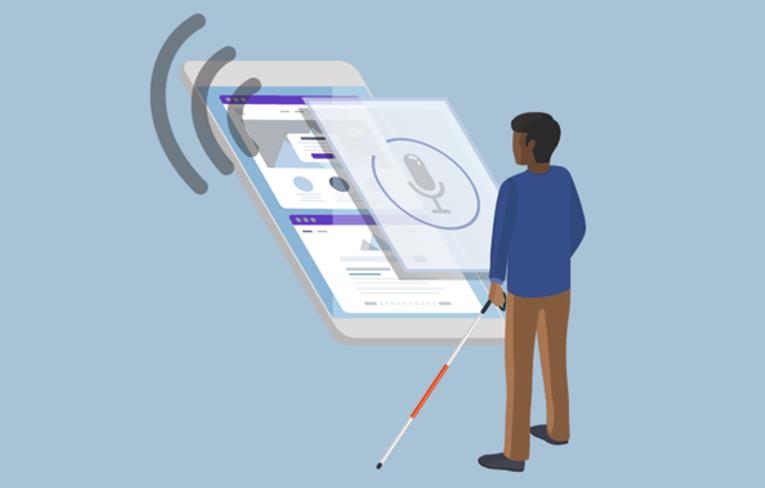
The visually impaired population encompasses over 253 million people worldwide. For a significant amount of this marginalized group, public transport plays an important role in productivity, community participation, and independence. As the primary form of commute for residents worldwide, buses are notorious for their tardiness and lack features specifically for visual-impaired passengers. Most people who are blind or visually impaired experience difficulties in getting on the right bus or getting off at the right destination. These situations usually force them to depend on other people that assist them in activities close to their homes, or simply stay at home. Currently, there is only one smartphone application that passengers can use to navigate transportation in Montevideo, but unfortunately it does not include methods of supporting visually impaired people with informing them the location of the bus, the frequency or duration of a certain bus line, or when passengers arrive at their destination. Our solution aims to create a smartphone application with voice commands, vibration, and speaker features as an alternative to assist people with visual disabilities with their mobility in the public transport system. This solution will improve quality of life, minimize safety concerns, promote autonomous living, and ultimately empower the visually-impaired.
Low Cost MRI Compatible Olfactometer
Siddhant Bhat, Daniel Blacher, David Knopp, Jason Lee, Sage Min
Olfactory Dysfunction has a number of causes. The most concerning cause is the degeneration of nerves in the olfactory bulb. This can be a sign of neurodegenerative diseases such as Alzheimer’s or Parkinson’s disease, and is also an indicator of 5-year mortality. In 2019, 1 in 8 Americans over the age of 40 have some form of olfactory loss, and this number has increased drastically post COVID-19, as it is a major symptom of infection. There is a current need for standardized methods to screen for olfactory loss, and obtain a quantifiable diagnosis. Current hospital olfactometers are very expensive and carry a bulky footprint and hence they cannot be used. Creating an olfactometer that is low cost, MRI compatible, and can provide aerosolized stimulus in both research and clinical settings will allow for research to create a standardized means of olfactory loss diagnosis and treatment. Our proposed solution utilizes a variety of components to design a lower-cost olfactometer to screen easily for treating olfactory dysfunction. Through these components, our approach and solution includes an air pump that will push air through one tube to an odorant chamber and another tube leading to a valve to the air. Afterwards, the ambient air will be passed through the odorant chamber absorbing the odor and be passed through the HEPA filter to purify and cleanse from any bacteria that may be harmful towards the patient. Additionally, a flow meter will be attached to determine the pressure and concentration of the air that will be administered to the patient. Therefore, a controlled amount of odorant air can be delivered in intervals to the patient. Lastly, the odorant air will be received by the patient through the nebulizer mask. As the patient smells the odor, the magnetic resonance imaging (MRI) will be able to track their brain activity aiding us in understanding the problems with olfactory dysfunction. The solution is purely mechanical, making it simple to learn and use. Our solution is non invasive, cheap, effective, and very simple to emulate.
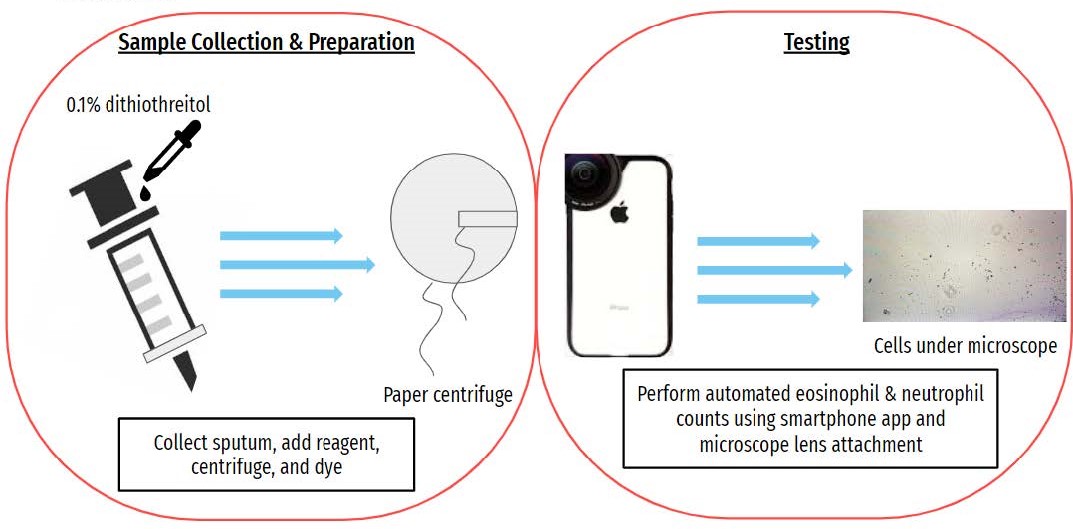
Low-cost Biomarker Monitoring for Chronic Pediatric Asthma in the U.S.
Lauren Ho, Ashley Kayabasi, Sam Pike, and Anisha Rath
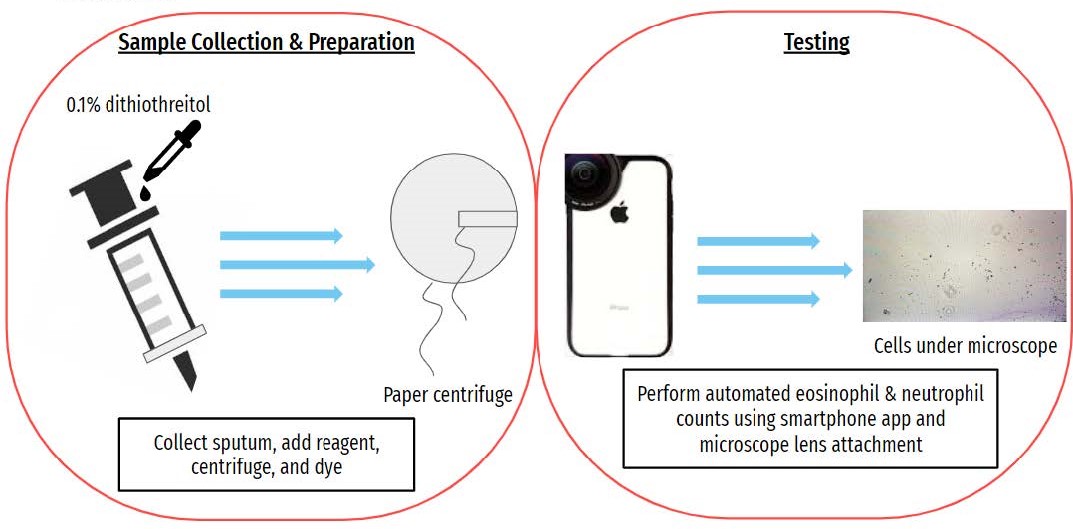
Asthma is a chronic immune disease that is characterized by inflammation and subsequent blockage of the airways. It is caused by a variety of stressors that include temperature, exercise, environmental triggers, infection, and others. Additionally, proper management of asthma entails numerous physician visits, especially for pediatric patients. Management techniques are determined by multiple testing methods such as questionnaires and spirometry. This makes the average cost of just asthma related physician visits a year over $700 per pediatric patient. Additionally, both questionnaires and spirometry do not actually measure the root cause: inflammation. Therefore, there is a clear need for an inexpensive and user-friendly device to properly monitor asthma biomarkers in children between the ages of 6-17 in the United States. Our solution is a point of care test which is able to measure the relative amounts of eosinophils and neutrophils in a sputum sample automatically using a smartphone app and microscope attachment. Sputum is collected willingly from the child and spit into a petri dish. The parent or user will perform the correct sample preparations using simple directions and the low-cost centrifuge. The smartphone will utilize a microscope attachment to perform an automated cell count. This test will provide patients' families the ability to measure critical biomarkers in a point of care setting while simultaneously giving physicians quantitative metrics that directly correlate to what the medications are treating. In turn, this will reduce doctor’s visits and increase management efficiency.
EpicPen: A Reusable, Replaceable Epinephrine Auto-Injector
Nathan French, Deepa Jayasankar, Brianna Shannon, Victoria Sinfield, Nick Will
Anaphylactic allergies can be fatal if not treated quickly and correctly with the administration of epinephrine. In the United States, 6 million people suffer from anaphylactic allergies with 3.6 million not readily equipped with an epinephrine auto-injector (EAI). Additionally, 56% of patients are concerned with the cost of EAIs, and 36% of patients are unable to afford one. It should be emphasized that the life saving drug epinephrine costs only $1, which is a fraction of the $636 cost of the EAI market-leader Epipen. Furthermore, EpiPen and other EAIs are designed to be single-use devices, meaning the entire mechanism must be replaced if used or when the epinephrine expires (every year). Therefore, there is a need to reduce overall lifetime cost for EAIs. Our project, EpicPen, aims to reduce cost by making the device both reusable and replaceable. For reusability, the team has designed a spring-loaded injection mechanism that allows the spring to be re-compressed for additional uses. For replaceability, the team has added a removable cap that allows access to the drug vial and needle for easy replacement. The design of the EpicPen allows for comparable ease-of-use and epinephrine viability to current devices on the market while incorporating novel features that will allow patients to be more readily equipped to treat their anaphylactic reactions at a lower lifetime cost.
Pepsin Fluidics: An Innovative Laryngopharyngeal Reflux Diagnostic Device for Accuracy and Patient Comfort
Aksana Doss, Shwath Kumaravel, Rhutuja Patil, Ali Senften, and Priyanka Seth

Laryngopharyngeal reflux (LPR) is a condition in which acidic fluid activates pepsin, a digestive enzyme which then regurgitates up to the level of the laryngopharynx (throat) and causes mucosal damage. Symptoms are typically hallmarked by sensations of post nasal drip, frequent throat clearing, hoarseness, issues with swallowing, a sensation of a lump in the throat, dry cough, and mucus in the throat. LPR is typically caused by reflux-enabling conditions such as an increase in abdominal pressure, gastroesophageal reflux disease, a hiatal hernia, or even a motility problem. Therefore, there is a need for a diagnostic device that can reliably measure pepsin levels so that patients may receive the proper diagnosis and treatment. The solution is composed of three parts: the mouth brace, microfluidic channels, and pH beads. The mouth brace is connected to the channels which have the pH beads incorporated inside it. Saliva is collected in the mixing chamber for 24 hours and the pH beads change to represent the concentration of pepsin. Figure 1a depicts the device prototype, featuring a flexible chip attached to the back portion of a mouth brace that holds the microfluidic channels held by dental wires which can be adjusted to improve fit. When applied, the mouth brace is placed over the top row of teeth and the microfluidic chip extends backwards towards the throat.
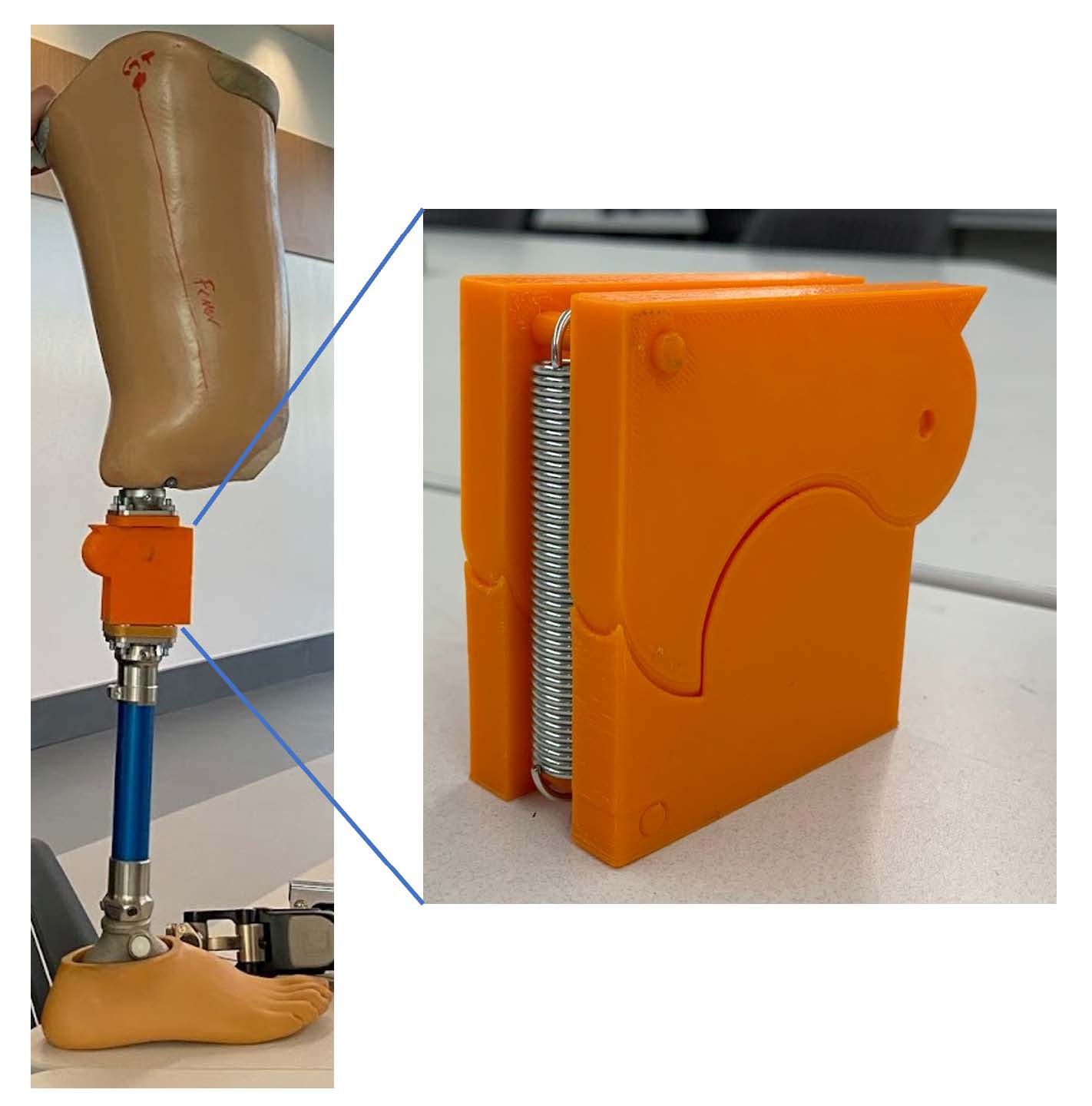
A low-cost mechanical prosthesis knee design to improve accessibility in low-income populations
Jeffrey Fang, Brandon Ruge, Anders Johnson, Patricio Figueroa, Billy Freudenthal
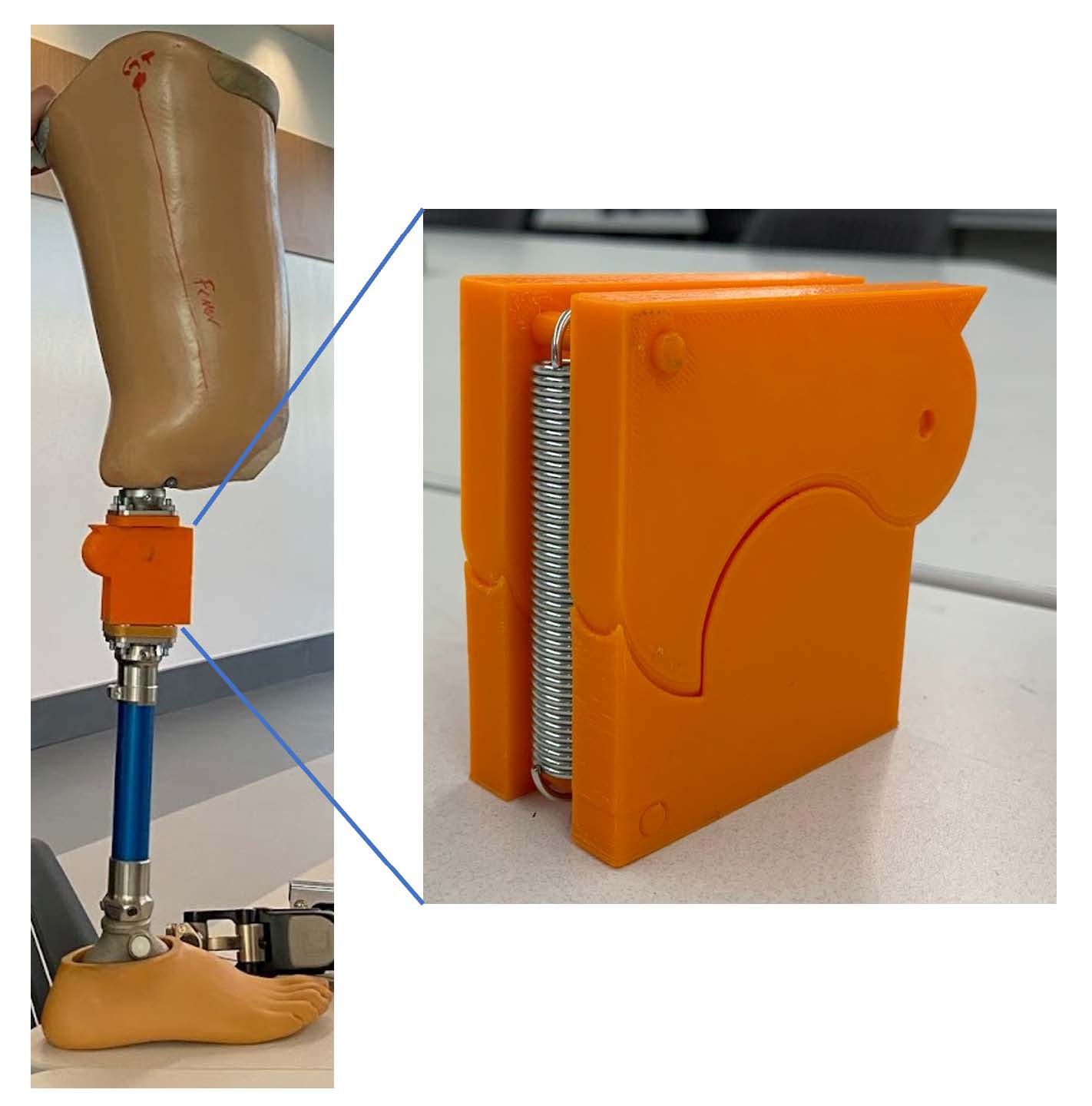
In third-world countries, access to low-cost knee prostheses that supply functionality to the user is an issue that needs to be addressed. These people may suffer limb loss due to vascular disease, trauma, or cancer; they cannot afford to pay for an at least $6,000 prosthesis with an average daily income of $2, and insurance often does not cover prostheses. Our knee prosthesis must give the user at least 115 degrees of use, withstand the user’s weight, and provide a walking experience comparable to knee prostheses on the market in the United States. Our solution incorporates a single-axis joint with a specific geometry that mainly ensures a securely locked standing position. On top of this, our prosthesis provides a natural gait while walking and delivers a comfortable experience for our users. This is achieved by the shape of the contacts on either side of the joint which hold a significant portion of the weight and allow for smooth movement within the desired range. What makes our proposal innovative is its low cost and simple design; the design is bioinspired and different from the popular bar linkage knee joints. When compared to other knee joints on the market, our knee joint is a simplification of other designs while achieving a similar user experience. The most attractive aspect of our knee is its low price and easy access for patients due to the use of a cheaper material and less material that comes with a simplified design. Our knee prosthesis will provide doctors in third-world countries with a cheap and effective way to help their patients with upper leg amputations live closer to normal lives. For amputees, receiving a prosthesis can be life-changing. In our case, a knee prosthesis will help patients with standing, walking, sitting down, and other daily activities. Aside from helping the patient, this innovation will impact medicine for low-income individuals. Patients in need or third-world countries will have the opportunity to receive a knee prosthesis they can afford.
Near-infrared (NIR) imaging used to detect nerve health
Ben Dahl, Jack Guo, Connor Hill, Sai Pothireddy, Lindsay Wright
An estimated 20 million Americans have some degree of damage to their peripheral nerves. This damage is clinically known as peripheral neuropathy, and it often results in an individual experiencing debilitating pain, muscle weakness, decreased sensations, and loss of autonomic processes such as sweating. Surgery is required for severe cases of neuropathy, and during peripheral nerve repair surgery, the surgeon resects the nerve until bleeding occurs and then proceeds to repair the nerve. Damaged nerves do not receive sufficient blood flow, so bleeding serves as a rudimentary visual benchmark that the surgeon has found the healthy portion of the nerve. However, in the case that more of the nerve is resected than necessary, there can be complications like longer recovery times, weaker signals propagated along the nerve, and the formation of painful neuromas. On the other hand, resecting too little nerve can result in the graft not being accepted by the native nerve. Thus, there is a need for a device that can accurately distinguish between healthy and damaged nerves during a surgical procedure; there is currently no device on the market that can accomplish this.
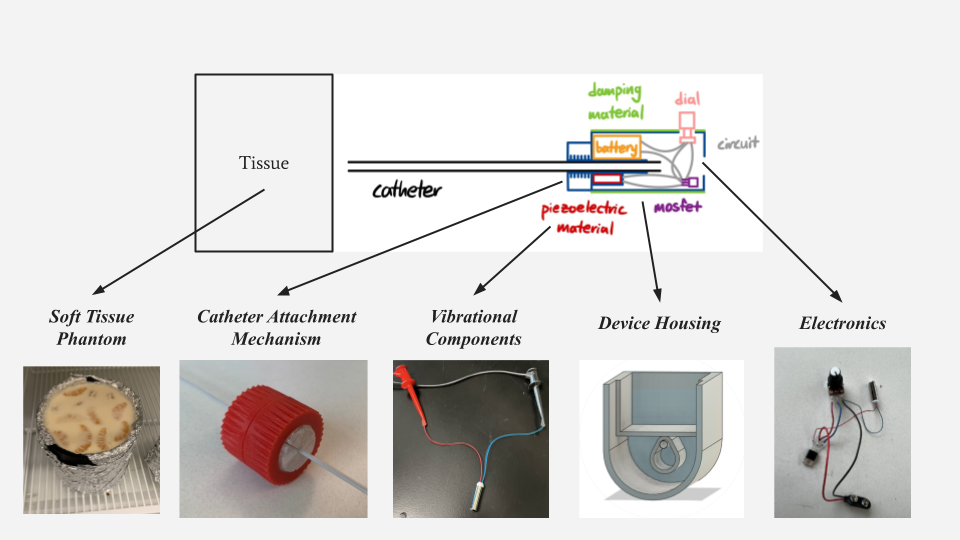
Design and Feasibility of Novel Peritoneal Dialysis Catheter to Prevent Mechanical Dysfunction in Neonate Patients
Kaitlyn Clapper, Muira Fontaine, Nina Render, Madeleine Stanik, Siting Zhang
Peritoneal dialysis is the preferred treatment method for neonates (0 - 1 year) presenting with acute kidney injury and end-stage renal disease. There are major complications associated with the use of current peritoneal dialysis catheters in neonates, including migration, occlusion, infection, and leakage. The prevalence of adverse events is further exacerbated by the unique challenges among the pediatric population, such as low birth weight, cardiovascular instability, limited respiratory capacity, tissue fragility, and lack of appropriately sized neonatal catheters. Adverse events leading to unnecessary reinterventions augment patient risk of an already highly vulnerable patient. There is a strong clinical need to increase the patency of current peritoneal catheters for use in neonatal patients.
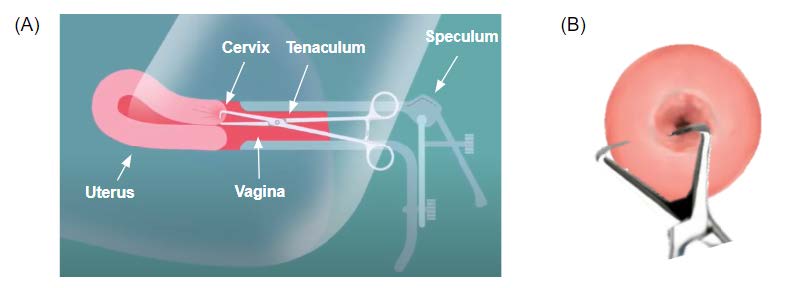
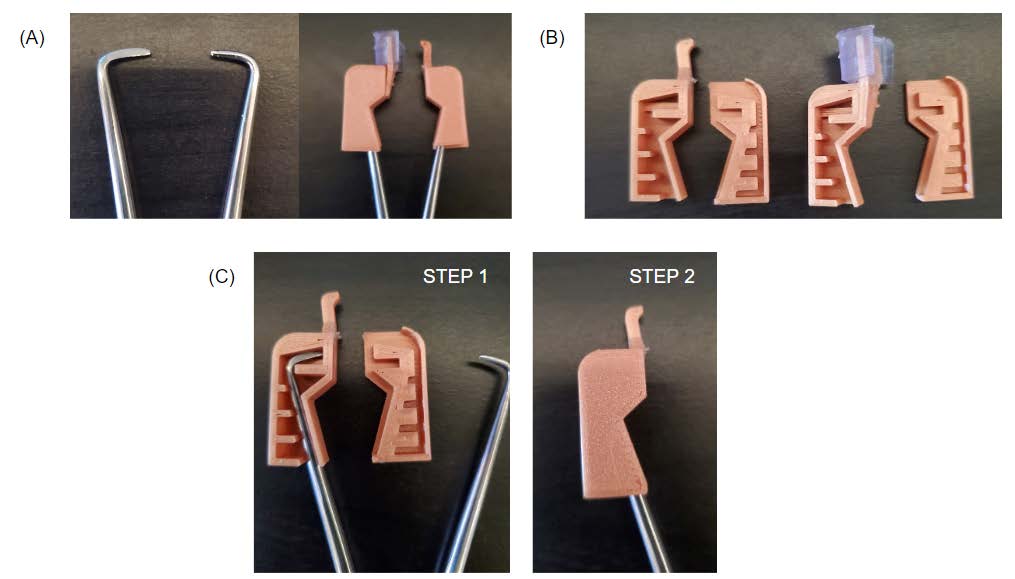
Atraumatic Cervical Clamp to Reduce Pain & Bleeding Associated with IUD Insertion Procedure
Anuya Kawathekar, Ashley Molnar, Haripriya Sakthivel, Katie Kisker, Maggie Craig
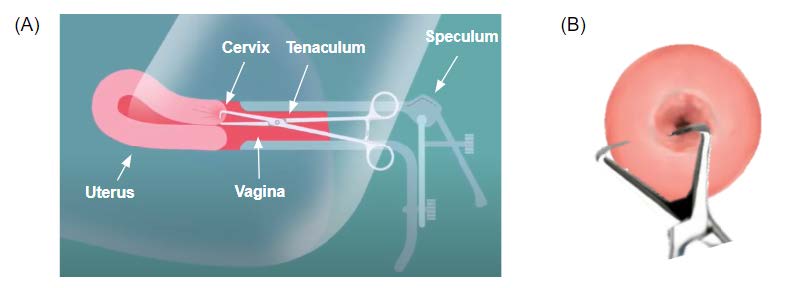
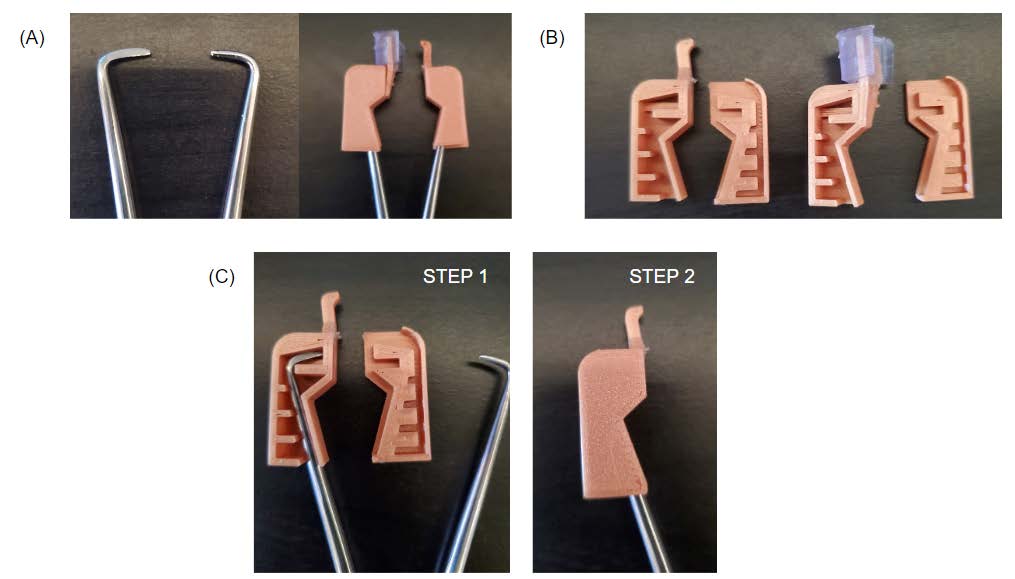
An estimated 20 million Americans have some degree of damage to their peripheral nerves. This damage is clinically known as peripheral neuropathy, and it often results in an individual experiencing debilitating pain, muscle weakness, decreased sensations, and loss of autonomic processes such as sweating. Surgery is required for severe cases of neuropathy, and during peripheral nerve repair surgery, the surgeon resects the nerve until bleeding occurs and then proceeds to repair the nerve. Damaged nerves do not receive sufficient blood flow, so bleeding serves as a rudimentary visual benchmark that the surgeon has found the healthy portion of the nerve. However, in the case that more of the nerve is resected than necessary, there can be complications like longer recovery times, weaker signals propagated along the nerve, and the formation of painful neuromas. On the other hand, resecting too little nerve can result in the graft not being accepted by the native nerve. Thus, there is a need for a device that can accurately
distinguish between healthy and damaged nerves during a surgical procedure; there is currently no device on the market that can accomplish this.
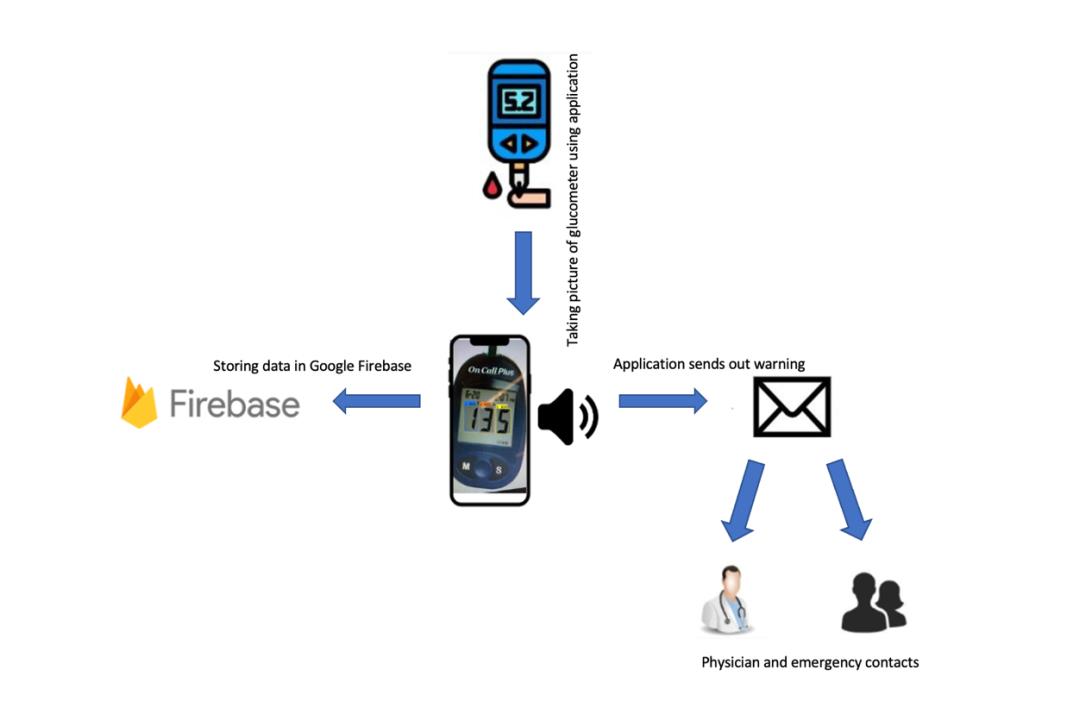
iOS Application for Visually Impaired (Total or Partial) Diabetic Patients that provides Audio Readouts of Glucometer Readings
Ally Cui, Lindsey Anoubon Momo, Edward Hsu
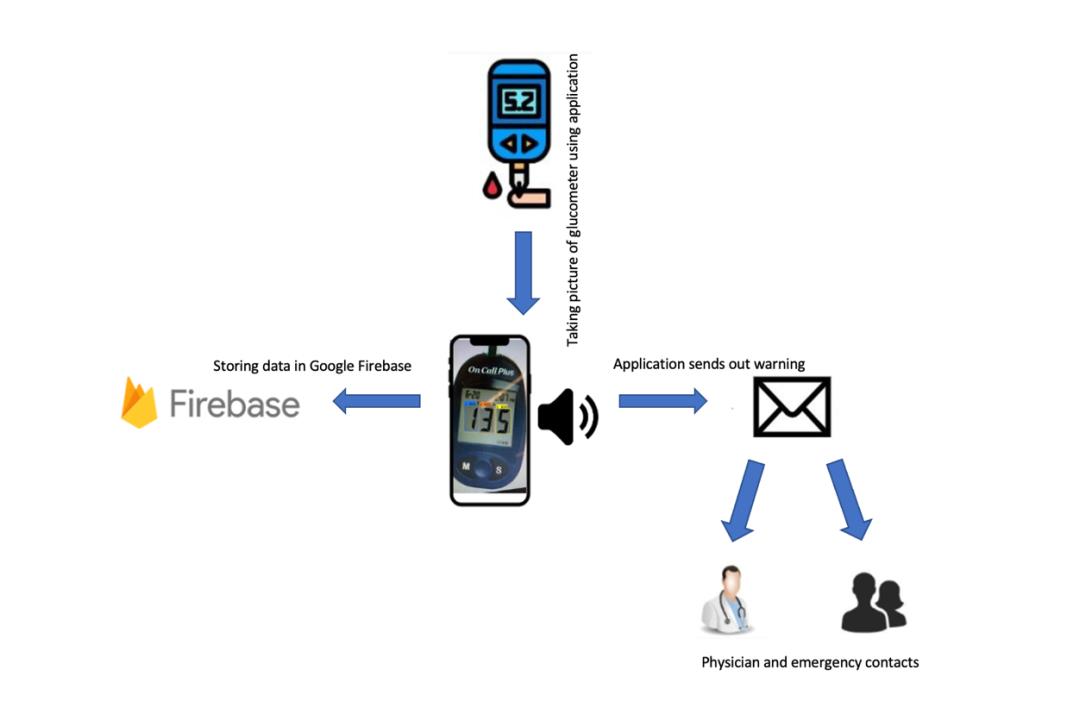
Currently, the global population with diabetes mellitus is approximately 463 million [1]. Diabetes retinopathy (DR) is a common complication of diabetes that could start developing during prediabetes and might lead to partial vision loss or blindness if left untreated [2]. The global prevalence of DR is 22.3%, which is around 103.12 million people. Such a number is estimated to be increased to 160 million people by 2045 [1]. Since diabetic patients are often required to measure and record their blood glucose levels regularly, patients that are partially or fully visually impaired would need additional assistance in taking such measurements. The current method for visually impaired, diabetic patients to know their glucose level would require the use of an audible glucometer or having someone assist them when they were taking the measurement, which are oftentimes expensive, inaccessible, and inefficient. Glucometer pricing varies based on their functionality, and audible glucometers are generally more expensive when compared to normal models. Moreover, this difference in pricing is greater in other countries. For example, in Uruguay, a normal glucometer kit costs around $35 - $45. However, audible glucometers would cost more than $300 [2]. While the cost of an audible glucometer in Uruguay is around six times the price in the US, the average annual income in Uruguay is 40% of the average annual income in the US [3]. Therefore, there is a need for a method that allows visually impaired patients to take their blood glucose measurements at a cheaper cost. The method should be capable of speaking out the blood glucose level of the patient with 95% accuracy. In addition, the method should also be able to record and store more than one hundred blood-glucose measurements (~two weeks of data). Lastly, the method should provide a warning to the patient’s emergency contacts if the measured result is out of the normal range (70 - 130 mg/dL before meals and less than 180 mg/dL after meals) [4]. This project is proposed by the University of Montevideo and aims to provide a novel smartphone application that works in conjunction with current, affordable glucometers on the market in Uruguay to deliver audible readings of blood glucose levels to diabetic patients that are visually impaired. This application’s audible readings will ultimately require less manpower to constantly watch over a diabetic patient. A real-time database can be easily accessed within the app, thus presenting a visualization of trends (Google Firebase feature). Communication efficiency will also be improved through the feature that notifies emergency contacts in case of a crisis. Data safety and privacy will also be considered through the secure storage of various blood-glucose measurements in Google Firebase and an initial login portal.
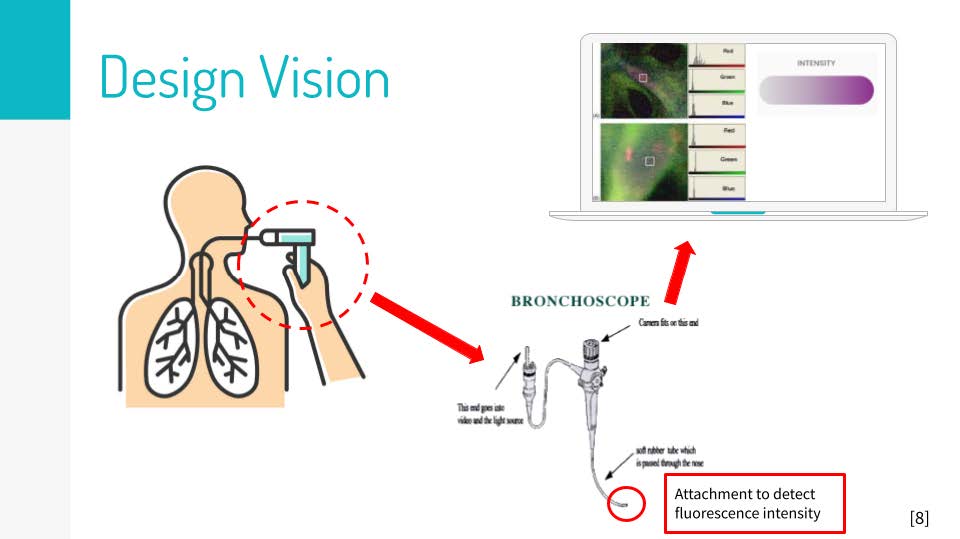
The Fiberoptic Bronchoscopy System for Detection of Aspiration Severity
Mitchell Jones, Shreya Kurdukar, Sreeram Nagappa, Anjali Parmar, Aditya Sathyaprakash
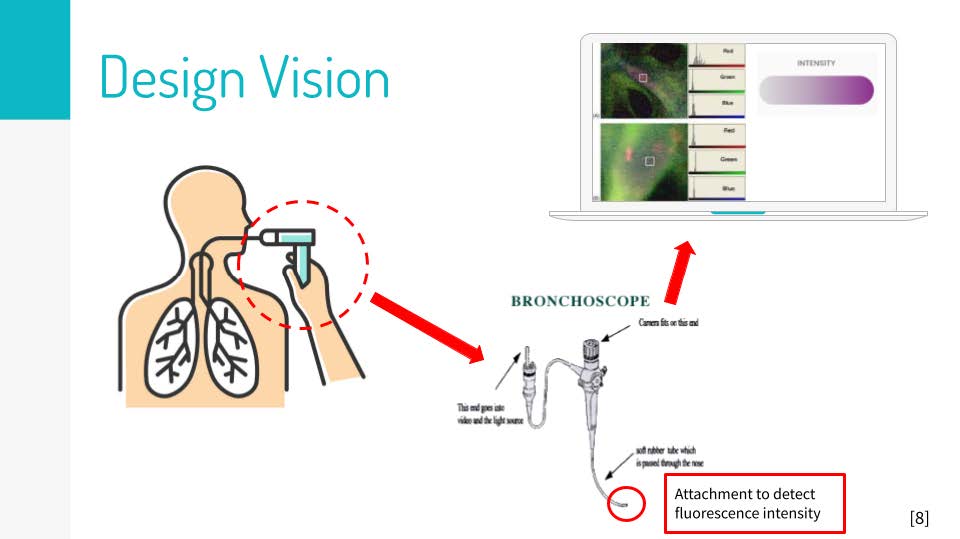
Aspiration is a medical condition characterized by the involuntary inhalation of foreign objects into the airway or the lungs, resulting in harmful consequences, such as pneumonia and acute lung injury. This issue is exacerbated in pediatric patients, whose smaller tracheas make it more difficult to diagnose inhalation abnormalities. Current technologies, such as videofluoroscopic swallow studies and fiberoptic endoscopic evaluations of swallowing, are able to collect visual information identifying the presence of aspiration. However, these technologies are unable to quantify the severity of aspiration. Thus, a method to quantify the degree of aspiration is needed in order to increase detection specificity during aerodigestive procedures and thereby reduce the risk of potentially dangerous sequelae. To address this need, our technology uses three primary components: an ingestible fluorescent dye, an emission/excitation bronchoscope system, and a quantification software (shown in Figure 1). First, patients will swallow a fluorescent dye which, when aspirated, will stain surrounding tracheal epithelial cells. Then, a white-light bronchoscope with an attached excitation optical filter will be passed through the trachea to excite the dyed epithelium. An emission receiver system (consisting of optical, phototransistor, and electrical filter technology) will receive and measure the intensity of the dye’s fluorescence as a voltage signal. Finally, the voltage signal will be converted into a measurement of intensity via software analysis. In the clinical setting, medical providers can use this system to get real-time results quantifying the severity of aspiration, thus helping them provide patients with more targeted treatment.
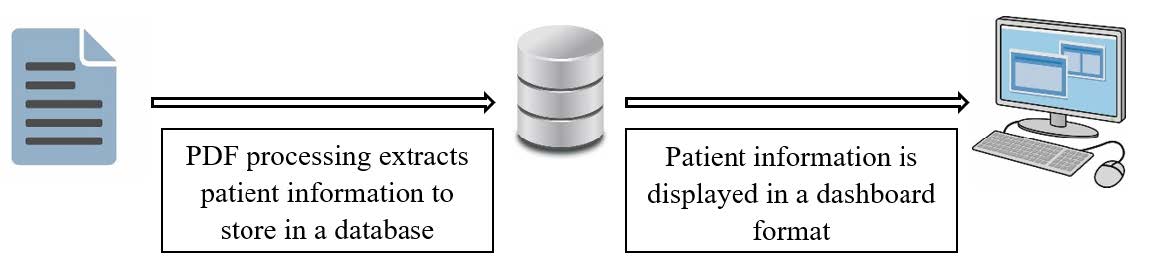
InManage - Inpatient Rehabilitation Management System
Marya Aldoukhi, Alexa Eby, Abhinav Prasad, Aletea vanVeldhuisen
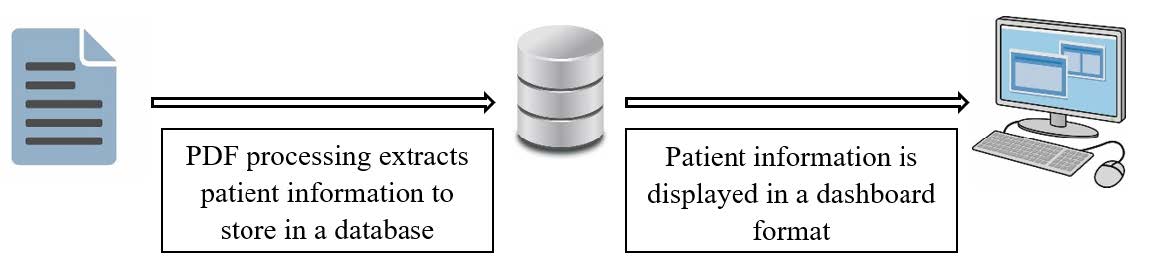
There are an estimated 2.4 billion people in the world who are in need of rehabilitation, with this number expected to increase in the coming years. The current referral process involves downloading PDF referral documents, reviewing them, and then manually entering the patient information into an electronic medical record (EMR) system. As a result, the referral process is non-standardized, lengthy, and time consuming. Our solution will provide a web-based application that processes PDF rehabilitation referrals and organizes the information to help admissions personnel make decisions about referred patients quickly and efficiently. Our solution will include accurate PDF information processing, a patient information database, an easy-to-use dashboard design, and login and data protection to ensure that patient information remains confidential. Our novel approach to medical information processing can breach the gap between EMR systems and eliminate the initial processing time for rehabilitation referrals across different EMR systems, minimizing time and error made in current procedures.
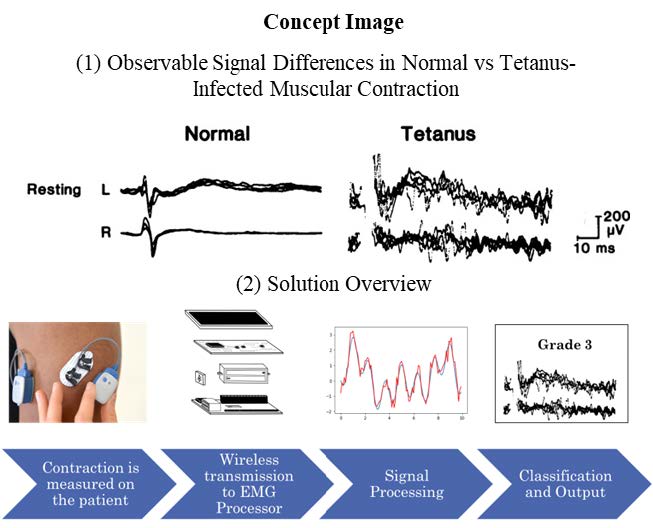
Electromyographic Classification of Tetanus in Low Resource Settings
Mary Lang, Tyler Williams, Tim Braun, Adalyn Meeks, Chris Shr
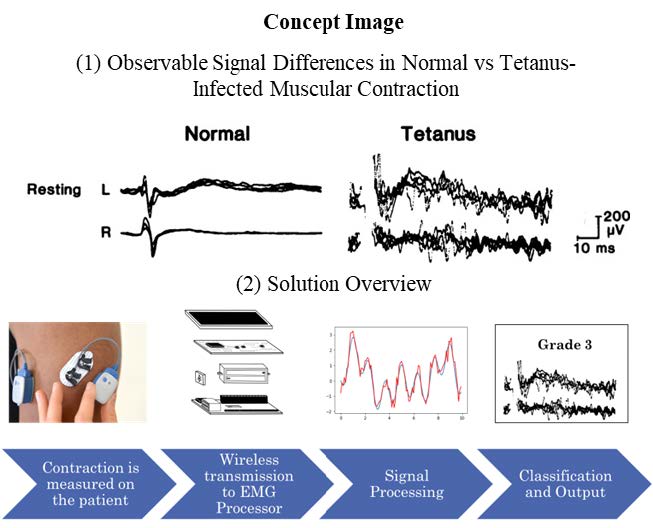
In low-resource settings, tetanus is a highly fatal disease, with mortality rates ranging from 20-70% [1]. Tetanus is initiated through infection with the bacterium Clostridium tetani (C. tetani), which secretes chemicals into the bodily system, inducing tetanus’s characteristic clinical symptoms of involuntary muscular spasms. Eventually, muscular spasms spread into the critical organ systems and cause death by respiratory distress. There is no current device or method on the market for the definitive diagnosis and subsequent classification of tetanus other than a physical examination of symptoms [2]. Empirical disease classification would be of value in the clinical care setting to determine if treatment regimens are effective in controlling symptoms and guiding patient care. There is a need for a device or method that can clinically determine the severity of tetanus in a patient. Some investigations suggest that the use of electromyography (EMG) can be useful in the monitoring of disease due to its inherent noninvasiveness, low cost, safety, and real-time feedback [3]. We propose a diagnostic solution utilizing wireless EMG signal acquisition paired with a classification algorithm that will be able to measure the involuntary muscle contractions caused by tetanus and provide instantaneous feedback to the physician in terms of disease progression. This solution should be accessible to low-resource settings in terms of usability as well as cost. A diagnostic solution using EMG technology would decrease the burden of the disease on both patients and physicians and assist in resource allocation in intensive or emergency care, particularly in low-resource settings. This solution would increase the accessibility of diagnostic tools for preventable diseases and direct more effective treatment for health-care centers in low-resource settings.
Mucus Protein Biomarker Detection for Diagnosis of Chronic Rhinosinusitis
Zach Lamantia, Jagroop Singh, Aika Patejdl ,Thea Nikolaou, Grace May

Chronic rhinosinusitis, CRS, affects over 10% of the adult population in the U.S. and Europe. CRS is characterized by chronic inflammation of the mucosa in the nose and paranasal sinuses where patients have symptoms such as nasal discharge, facial pain, congestion, and lost or reduced sense of smell. Recently biological therapies have provided an additional treatment option to otherwise uncontrolled CRS in patients. In these therapies, monoclonal antibodies target specific type 2 inflammatory proteins commonly found at elevated levels in patients with CRS. Unfortunately, clinicians are not able to select the most effective biologic treatment for patients since there is no test to determine which inflammatory protein is elevated in each patient. Therefore, the patients go through a process of trial and error where they try different biologics for 6 months at a time until a beneficial treatment is found. Not only does this process prolong patient discomfort for months or years, this is a very expensive process since biologics cost around $37,000 per year. Thus, there is a need for a simple, inexpensive, sensitive, point-of-care device that can accurately indicate which protein biomarker is elevated in a CRS patient, and therefore which therapy they should select. To address this need, we designed a novel lateral flow assay (LFA) platform that detects levels of IgE (one protein that could be elevated in a CRS patient) from a patient’s mucus sample. This LFA takes less than 30 minutes to run including sample collection, detects levels of IgE at or above 50 ng/mL, costs less than $10 to manufacture, and has a testing procedure that takes less than one minute to understand. With our lateral flow assay design, clinicians have the power to revolutionize the standard of care for CRS patients across the world by bringing the wait time for the correct therapeutic from at least 6 months down to just 30 minutes.
An Automated Method for Classifying Unhealthy vs Healthy Nerve Tissue in Open-Surgey Applications
Kevin Bautista, JP Lamia, Kevin Cragg, Tom Lee, Sradha Ravishankar
Proper surgical treatment of transected peripheral nerve tissue requires sufficient removal of the damaged area prior to utilizing common repair options like nerve grafts. Currently, surgeons are limited to their operating experience when identifying healthy from unhealthy nerve tissue based on nerve texture and resulting blood flow, thereby taking minutes to properly detect and remove unhealthy nerve tissue. Failure to remove damaged nerve tissue before surgical treatment can result in neuropathy, insufficient recovery, limited sensation, and the formation of painful neuromas in the extremities. To enable surgeons with a better means of characterizing nerve tissue, a device capable of rapidly classifying healthy from unhealthy nerve tissue is needed.
Temperature Control for Blood in Transport with Thermoelectric Cooler (TEC)
Maya Alborn, Kyle Chang, Kyndall Davis, Trevor King, Jiyuan Yang
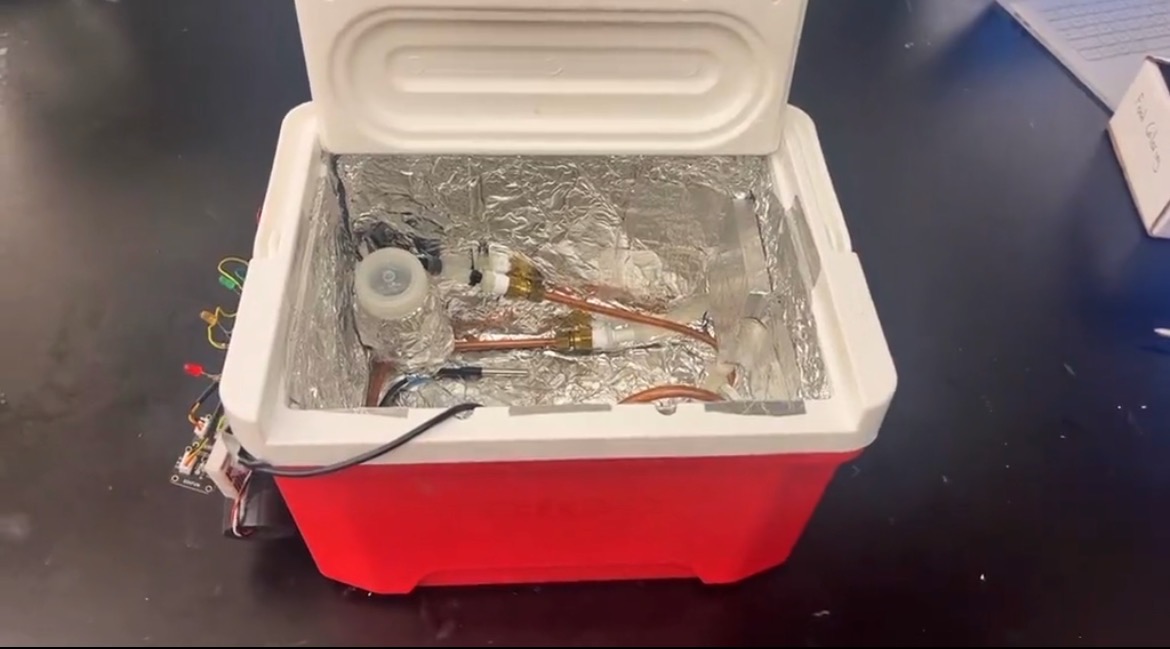
A current challenge in the blood supply chain is maintaining the temperature of blood products between 2-6°C to increase the blood viability. To address this need, the solution will utilize a cooler with coolant distributed throughout attached to a thermoelectric cooler unit and arduino circuit to create a closed loop system to monitor and correct the internal temperature of the device. This solution innovates over current solutions because all current products on the market use ice or other coolants to try and maintain temperature, but do not contain any temperature monitoring components and require a person to interact with the device in order to cool it back down to the proper temperature while our device will cool off completely on its own assuming it has enough power. With this new device in the market instead of current solutions, there should be a large reduction of blood waste of red blood cells and plasma due to improper temperature control.
Low-Cost Upper Limb Prosthetic for Tanzania
Moyo Shobowale , Shreyas Varathan, Halle Von Ah, John Picucci, Amber Carpenter

There are over 16 million amputees in Africa, which covers about 24.6% of the amputees globally. Specifically, most upper limb amputees come from birth defects, automobile accidents, and onsite work accidents. Unfortunately, the average cost of a myoelectric prosthetic is $20000 to $100000 USD, while the average annual income in Tanzania is around $1020 USD. The goal of this project is to create an affordable myoelectric prosthetic utilizing 3D-printing technology that costs less than $500 USD: an accessible price for the general Tanzanian public. To ensure that our solution is viable for our target population our prosthetic design will include features such as an EMG interface, 360° servomotors, fishing line, Acrylonitrile Butadiene Styrene (ABS) material, etc. Our group is partnering with RoverLabs, a prosthetic company based in Tanzania, to develop a product that is unique from their Mkono-1 prosthetic. Our prosthetic is innovative compared to the Mkono-1 due to its affordability; the Mkono-1 is about 5000 USD, while our product will be about 500 USD. Our solution will increase the general populous access to high-functionality prosthetics, due to its affordability, which in turn will increase the able-bodied workforce.