2015 Senior Design Projects
kiKNEEsio Adaptive Brace -- Adapting to your ACL rehabilitation needs
VAPscent: Diagnosing Ventilator Associated Pneumonia via Exhaled Breath Analysis
The Amblemotion Project: A Low Cost, Lower Limb Prosthetic for Guatemala
SAVED: Rapid Administration of Care for Combat Wounds
Regeneration of Muscle via Electrical Stimulation and Extracellular Matrix
Going Out on a Limb to Provide Sensational Sensory Feedback
BabyStat - A Simple Tool to Combat the Complicated Issue of Low Birth Weight
Neural Magnetics: Noninvasive Peripheral Nerve Magnetic Stimulation
A Novel Screening Device for Detection of Early Stage Ovarian Cancer
Improving Hemodynamic Monitoring and Temperature Control during Anesthesia
Traumatech: Brain Injury Detection
kiKNEEsio Adaptive Brace -- Adapting to your ACL rehabilitation needs
Jane Liao, Morgan Saras, Alex Lewis, Kaitlyn Jarry, Adhit Ramamurthi
With a recent rise in sports and physical activity participation amongst youth and young adults, more injuries have been reported between the ages of 15 and 24 years. The knee is the most vulnerable and injury-prone joint, with Anterior Cruciate Ligament (ACL) tears accounting for upwards of 200,000 injuries per year for this age group in the United States alone. This poses a problem because the ACL alone provides 90% of knee joint stability.
The purpose of our solution is to provide a knee brace used during ACL reconstruction recovery to inform patients and clinicians of knee ranges of motion while providing adaptable levels of support during exercise. Compared to current brace solutions, this solution innovates by providing multi-level of support, containing real-time electric feedback, and offering detachable components for personalized support. An underlying compressive mesh supports the knee from all directions. External hinges inhibit unsafe ranges of motion such as hyperextension and internal tibial rotation via mechanical limits. Electronics integrated into the hinges measure joint angles and provide vibrational feedback when the user encroaches upon unsafe motions. Lastly, detachable elastic components mimic joint taping techniques to support specific knee structures necessitated by each patient’s rehabilitation program.
Bench tests including material fatigue, range of motion, and compression pressure have verified the device meets specifications for withstanding repeated use, preventing unsafe knee movements, and providing support and pain relief. Additionally, electrical components have been proven to calculate joint angles within 2 degrees and to deliver vibrational feedback and numerical data to a user-friendly iPhone application for tracking progress. In conclusion, the kiKNEEsio Adaptive Brace provides adaptable levels of support while supplying range of motion feedback and data to the user. This will, in turn, reduce the rate of re-injury during exercise following ACL reconstruction and allow for quicker return to activity.
VAPscent: Diagnosing Ventilator Associated Pneumonia via Exhaled Breath Analysis
Jade Tang, Anna Woodson, Kaitlyn Mast, Lindsey Gengelbach
One of the most prevalent hospital acquired infections is ventilator associated pneumonia (VAP). Up to 300,000 cases of VAP per year occur in the U.S. alone. This is especially concerning because the current diagnostic methods for VAP are invasive, time-consuming, expensive, imprecise, and may lead to additional risk factors for the patient. In fact, studies have shown that inadequate therapy during the initial 48 hours of VAP can lead to a mortality rate of 91%. Staphylococcus aureus causes 33% of all VAP cases, thus earlier diagnosis of S. aureus can mean earlier treatment for an already vulnerable patient population. Our novel solution is an electronic sensor that attaches directly to the existing ventilator tubing. The sensor has an internal heated component, which changes resistance based on the amount of ethanol present in exhaled breath of the patient, thereby signaling the presence of the bacteria. The sensor continuously records and reports data quantitatively in a user interface with a built in alarm system so that a confident diagnosis can be made. Our solution is able to detect ethanol produced by S. aureus in exhaled breath noninvasively with sensitivity and specificity of 95% in a model ventilator circuit. Initial detection of VAP can be made approximately six hours after an infection of S. aureus is present. This is 66 hours faster than the average VAP diagnosis time of 72 hours! Earlier detection of S. aureus leads to more effective treatment because healthcare professionals will not need to differentiate bacteria type by culture, therefore, appropriate antibiotics can be administered right away. These antibiotics can begin fighting off infection, which increases the chance of patient survival while decreasing the massive patient costs associated with extended hospital stays.
The Amblemotion Project: A Low Cost, Lower Limb Prosthetic for Guatemala
Jynx Boyne, Jim McCarthy, Fahim Rahman, Ana Valenca, Sarah Young

Lower-limb amputation is prevalent throughout the world. However, current prosthetic legs are far too expensive for those in developing countries. Currently, the Range of Motion Project (ROMP), a non-profit organization, provides low cost prosthetics to Guatemalan amputees, but the organization relies heavily on donated devices and materials. These donations are unreliable, often improperly sized for the population, and rarely include prosthetic liners. Therefore, the goal of this project is to provide ROMP with a method for creating lower limb prosthetic components that reduces their dependency on donations. Amblemotion has designed lower limb prosthetic components (foot, pylon, socket, and liner) that can be manufactured for less than $350 (estimated) total. This was accomplished through designing a solution that can be manufactured from ROMP’s current equipment, and incorporates locally available materials. In addition this solution provides innovation through an adjustable socket, a pylon made from recycled bicycle parts, and repeatable manufacturing processes for creating a liner and correctly-sized foot. The solution has passed structural and longevity testing per ISO 10328, demonstrating device safety during patient use. Additional testing has been completed to ensure all solution components can be manufactured at ROMP facilities. With this project, Amblemotion has successfully provided ROMP with a low-cost lower limb prosthetic device that can be reliably manufactured on site. This solution will ultimately allow ROMP to provide more comfortable and appropriately sized prosthesis to their current patients and reach a larger population of amputees in Guatemala.
SAVED: Rapid Administration of Care for Combat Wounds
Spencer Chiang, Paolo Lacanienta, Peter Marshall, Tyler Mayrosh, Will Voors
Every year, soldiers die of survivable junctional hemorrhagic wounds because they do not receive immediate medical treatment in time. Currently, many of the ‘gold standard’ first aid devices such as tourniquets and gauze cannot adequately treat severe junctional penetration wounds quickly and effectively. Soldiers are in need of a quick, one handed, effective device that can stop bleeding in any number of penetrating wounds received. Current solutions do not achieve this since they address a single type of wound at a specific anatomical location. Our revolutionary solution for this problem is the application of a multi-use pressure assisted syringe that contains a coagulant media to prevent further bleeding through direct pressure and immediate activation of the clotting cascade. What sets the Self-Administered Vascular Exsanguination Deterrent (SAVED) device apart from other delivery devices is the innovation in efficiency, reusability, and ease of use. The device works by injecting a coagulant doped material into a high velocity projectile wound; the coagulant and material provide both local coagulation and direct pressure onto the site of the wound. The SAVED can be self-administered with one hand and used up to three times per reloadable cartridge that allows for a simple and fast removal of the coagulant after use. Through rigorous testing of simulated penetration wounds, the device demonstrates that it can be quickly administered and prevent the overall blood loss from a wound leading to exsanguination. The SAVED accomplishes the 15 second blood loss prevention as boasted by the leading competitor while providing an ergonomic body for self-administration and a multi-use design. The SAVED will be able to provide the temporary care that is crucial in a combat situation. The introduction of this device into the standard issued equipment of soldiers, law enforcement and emergency responders will result in countless lives being SAVED.
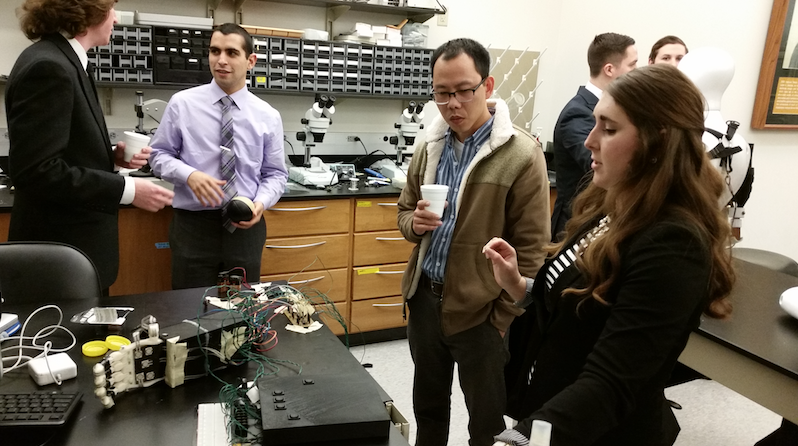
Regeneration of Muscle via Electrical Stimulation and Extracellular Matrix
Victoria Messerschmidt, MacKenzie Tweardy, Melanie Venderley, Lauren Williams
Approximately 60% of military veterans returning from duty suffer from volumetric muscle loss (VML) after experiencing a traumatic event affecting one or more extremities. In total, there are over 10 million sufferers. Due to the permanent disruption of muscle regeneration, VML leaves the injured person with an excessive amount of scar tissue at the trauma site, resulting in a severe lack of functionality. Clinical standard of care does not exist for this debilitating disease; therefore, a new device is required to regrow fully functioning skeletal muscle. An innovative solution has been developed utilizing a combined approach of highly-researched areas within tissue regeneration and electrical stimulation. The device is composed of a scaffold and muscle stimulator. This innovative scaffold combines biological materials that have never before been integrated - a decellularized extracellular matrix and hyaluronic acid gel. Additionally, the muscle stimulator is made of stainless steel electrodes to apply electrical fields, supplied by a microcontroller, for accelerated and proper alignment of muscle growth. The novel combination of the scaffold, cells, and stimulation have contributed to the formation of in vitro muscle formation which responds in a viscoelastic manner, similar to that of natural physiological muscle. This novel solution, used to treat the debilitating effects of volumetric muscle loss, has led to significant contraction and alignment of muscle fibers. The expected results will show that the circuit and program accurately stimulate the cells, producing proper skeletal muscle alignment. It will also show that muscle cells attach and proliferate in the scaffolds. All of the results have met the developed design specifications and show that this innovative device is capable of treating VML. With the implantation of this device, the lives of military veterans would vastly improve the quality of life in comparison to today’s standards
ClotCapture: Reduction and Removal of Blood Clots within an Extra Corporeal Membrane Oxygenation Circuit
Danielle Messman, Mary Christy, Kelsey Bayer, Ryan Watts
In the last six months of 2015, there have been over 70,000 patients on Extra Corporeal Membrane Oxygenation (ECMO) therapy for days, weeks, or months at a time. ECMO is a heart-lung bypass machine that is used in order to pump and oxygenate blood manually for patients who are experiencing heart and/or respiratory failure. It is commonly used as a bridge-to-transplant or surgical support for newborns and adults. A common problem that arises during ECMO use is the formation of blood clots within the circuit tubing at points of connections or turbulent flow. If one of these clots breaks free, it can either cause thousands of dollars’ worth of circuit component replacement costs or travel into the patient's body and occlude major arteries causing potentially life-threatening consequences. Currently, there are only chemically based solutions that cause just as many problems as they aim to solve. There is a need for a mechanical method for reducing the prevalence of blood clots in the ECMO circuit and removing these clots if they do form.
The design solution is an in-line filtration chamber that contains a membrane that can capture clots and be removed and exchanged if necessary. This device is unique in that it can keep the ECMO staff informed of the status of the membrane functionality through a user interface and alarm system based on feedback from in-line pressure sensors. The results are expected to reveal that the membrane and battery will have a week long life span while maintaining 85% of cardiac output before membrane and battery exchange is needed. The membrane will capture 95% all clots that have the potential to occlude major arteries. The device is expected to adhere to these expectations and in doing so will help tens of thousands of patients in the United States annually.
Lending a Hand: A Cost-Effective and Functional Above-Elbow Prosthetic Solution for the Developing World
Hannah Buvala, Chase Haddix, Abby Shaw, Dylan Sinks, Mary Towers, Patrick Zeid
Above-elbow prostheses tend to be complex and expensive, and accessibility of these devices is not always prevalent in developing countries. Approximately 80 percent of people with amputations live in the developing world and only about 2 percent have access to prosthetic care. The income of workers in these developing countries greatly relies on their ability to perform manual labor. It is important to solve the issue of a cheap, durable, and accessible upper-arm prosthetic device. To address this global need, a design has been created that will allow amputees to return to the workforce and improve their quality of life. The design focuses on a synergy of low-cost materials and intuitively simple mechanical systems that are easily reproduced in a developing country’s manufacturing setting. The prosthesis features a universal but adjustable socket which further simplifies production and lowers cost of the device. This innovative socket drastically reduces fitting times and increases the longevity of device lifespan for each user. The elbow allows for two planes of rotation, which is unique compared to most prosthetic devices currently on the market. The materials chosen for this device are low cost and widely-available in third-world countries, including heat-moldable polypropylene, PVC, and aluminum. To test the solution, the device was fitted to above-elbow amputees who performed precision and functionality validation tasks. Feedback from these volunteers indicates that the device is comfortable and effective as a low-cost option for returning natural function to upper limb amputees. If implemented correctly, this device will provide a viable prosthesis to a patient in need. In doing so, the need for repeated visits to limited privatized health care settings would be greatly diminished. The economic burden to low income patients will be reduced and allow the user to return to daily life.
Going Out on a Limb to Provide Sensational Sensory Feedback
Alex Hathoot, Ryan Koch, Colin Kuntz, Sabrina Scalf, Libby St. Clair
 The sensation of physical touch is often taken for granted. No second thought is given to picking up a delicate object without watching your hand or finding an item in the dark. However, when this sensation is absent, the effects are drastic and devastating. This loss of feeling is experienced by nearly 2 million amputees in the United States. Upper limb loss accounts for approximately 11.5% of all amputations, and more than 16,000 new upper limb amputations occur annually in the U.S. Many significant advances have been made in the motor control of upper limb prostheses, but sensory feedback remains largely unaddressed.
The sensation of physical touch is often taken for granted. No second thought is given to picking up a delicate object without watching your hand or finding an item in the dark. However, when this sensation is absent, the effects are drastic and devastating. This loss of feeling is experienced by nearly 2 million amputees in the United States. Upper limb loss accounts for approximately 11.5% of all amputations, and more than 16,000 new upper limb amputations occur annually in the U.S. Many significant advances have been made in the motor control of upper limb prostheses, but sensory feedback remains largely unaddressed.
Our design solution features 10 flexible, adhesive pressure sensors that will be arranged along the fingers and palm of any existing upper limb prosthesis. The sensors record pressure readings from the fingers and palm and transmit them to a processor. The patient also wears a stimulating shoe sole that is equipped with vibrational motors mapped to the sensors on the hand. When the patient touches or grasps an object, the corresponding motors in the shoe sole vibrate, delivering intuitive sensory feedback regarding the strength and location of the pressure felt by the hand.
The device meets numerous design specifications for battery life, safety, and functionality. The user will be able to distinguish between different levels of pressure on their prosthesis and the general location of the pressure in real time. This innovative solution will allow patients to interact with their environment in a way not currently afforded by any prosthesis available on the market. The low cost and the adaptability of the solution to the patient’s existing device will allow this product to reach as many patients as possible to help them regain sensations that once seemed permanently lost.
Temporary pulsatile assist device for acute left systolic heart failure - A solution that reevaluates the treatment of heart failure
Matt Geiser, Blake Milner, Emily Prus, Casey Schilling, Jake Wagner
 Heart failure is an incredibly prevalent disease with a yearly incidence of over 500,000 people in the U.S. alone. Acute left systolic heart failure is a condition where the left ventricle is suddenly no longer capable of ejecting the proper blood volume out to the body. This can be caused by various circumstances, some of which include infections, pulmonary embolism and heart attack. In order to fulfill the need for a less invasive and more effective solution for this condition, an implantable device for the left ventricle that improves cardiac output has been developed. Supporting and treating the heart during a case of acute heart failure could provide temporary cardiac support while physicians treat the underlying cause of potentially fatal failure.
Heart failure is an incredibly prevalent disease with a yearly incidence of over 500,000 people in the U.S. alone. Acute left systolic heart failure is a condition where the left ventricle is suddenly no longer capable of ejecting the proper blood volume out to the body. This can be caused by various circumstances, some of which include infections, pulmonary embolism and heart attack. In order to fulfill the need for a less invasive and more effective solution for this condition, an implantable device for the left ventricle that improves cardiac output has been developed. Supporting and treating the heart during a case of acute heart failure could provide temporary cardiac support while physicians treat the underlying cause of potentially fatal failure.
The device features an intraventricular inflatable bladder that attaches to the heart wall and is deployed through a minimally-invasive catheter. The bladder is inflated and deflated in time with the heart’s electrical rhythm by a pump. The inflation of the bladder provides pressure-driven flow of blood out of the compromised left ventricle and into the body in order to improve ejection fraction. The intended use of this device is for temporary use (<6 hours). Based on in situ testing using a model of the circulatory system, this device utilizes a minimally invasive delivery approach and significantly increases the ejection fraction.
This device fulfills a large gap within the market for a temporary aid for acute heart failure patients that assists the heart to eject the proper blood flow out to the body, unlike current devices which only decrease the resistance placed on the ventricle. In the future, studies should be conducted to apply this concept towards a long-term solution to treat heart failure permanently in addition to decreasing the severity of acute heart failure.
BabyStat - A Simple Tool to Combat the Complicated Issue of Low Birth Weight
Alex Carle, Charlotte Hoo, Ben Robinson, Stephanie Thiede, Mari Tomizawa
Low birthweight (LBW) is the leading cause of infant mortality and attributed to debilitating complications in surviving infants that can last into adulthood. For these reasons, there is an associated cost of $20,600 - $52,300 for each LBW newborn in the first year of life alone. Since LBW is primarily caused by non-physiological factors stemming from a mother’s environment or life choices, policy has potential to decrease the prevalence of LBW. Current efforts to reduce LBW are largely aimed at regulating behavioral risk factors; however, little has been done towards regulating pollution levels that contribute to increased LBW prevalence.
To make evidenced-based policy addressing issues of LBW, there needs to exist a public health surveillance system that can systematically utilize healthcare and environmental data to efficiently aid policy-makers in recognizing and addressing the issue of environmentally-caused LBW. The design solution is a software tool that allows policy makers to calculate the prevalence and impact of LBW at a county level. Using mathematical modeling, the tool identifies the leading environmental causes and economic impact of local LBW rates. The solution involves a friendly user interface, a back-end database to host data, and models to calculate the impact of environmental factors on LBW and the corresponding economic costs.
The solution is the first health surveillance system targeted at policy makers to monitor LBW and provide comprehensive modeling of the condition’s environmental causes and economic burden. Results achieved include the successful completion of a proof-of-concept software prototype that yielded user-satisfaction rates of 90%, modeled environmental correlation to LBW with 70% accuracy, and modeled economic impact with 70% accuracy. With widespread use by policymakers, the solution can bring about policy changes that will significantly reduce LBW and its social and economic burdens.
Neural Magnetics: Noninvasive Peripheral Nerve Magnetic Stimulation
Jesse Bucksot, Stephanie Cernera, Daniel Maruri, Sam Stukov
Vagus Nerve stimulation (VNS) is a well-tolerated therapy for drug resistant epilepsy patients. Currently, VNS is an invasive procedure, requiring an incision into the neck and clavicle. Transcranial Magnetic Stimulation (TMS) is a noninvasive alternative that uses magnetic fields and induced current to stimulate the brain, but it stimulates a larger area than desired. Repurposing TMS to stimulate the Vagus Nerve and other peripheral nerves could be beneficial for people suffering from epilepsy and many other neurological disorders. Noninvasive stimulation could improve the lives of thousands of people by eliminating the need for surgery, which can be incredibly expensive. The system would need to be a safe and efficacious device that a physician can easily use on a patient suffering from a neurological disorder. The proposed solution is a transdermal magnetic nerve stimulation device that uses modified TMS coils optimized for peripheral nerves. The coil is designed to obtain the necessary stimulation depth with a minimized stimulation area. The power supply creates a series of high intensity impulses at a low frequency to achieve the desired stimulation. The device has demonstrated that it is able to generate an electric field greater than 2 V/cm at a depth of 4 cm, which is the threshold electric field to cause a stimulus, and it has achieved a focused field of 15 cm2. The debut of Transdermal Magnetic Nerve Stimulation will have a tremendous impact in helping treat the 4 million people suffering from drug resistant epilepsy in the United States. Not only can this stimulation be applied to the Vagus Nerve, but also to peripheral nerves for conditions such as chronic pain and peripheral neuropathy. With this device, it will be possible to conveniently treat the millions of patients with selective neurological conditions in a noninvasive and highly effective manner.
TB or Not TB: An Innovative Gastric Collection Device for Improving South African Pediatric Tuberculosis Diagnosis
Jordan Addison, Amelia Adelsperger, Amy Koester, Daniel Romano, Julia Swartzenberg
Tuberculosis, a bacterial infection, primarily attacks the lungs, leading to intense fatigue and weight loss, a sputum-producing cough, and death. Of the 450,000 new cases of tuberculosis (TB) diagnosed in South Africa each year, approximately 15-20% occur in children. This pediatric subpopulation goes largely undiagnosed due to their inability to cough up a bacterial sample for conventional diagnosis. Currently, the two best techniques for obtaining this sample are sputum induction and gastric lavage, which are highly invasive, uncomfortable, and require clinical settings. A rapid diagnostic device, GeneXpertTM, is readily available in South Africa, but is useless for diagnosing pediatric TB without a bacterial sample. Because of the difficulties associated with obtaining these samples from children, there is a need for an inexpensive, intuitive, and non-invasive method of collecting GeneXpertTM-compatible bacterial genome samples. Therefore, our team has designed a solution that utilizes the body’s natural processes to collect a bacterial sample, eliminating the need for distressing procedures that require administration by trained clinicians. Our proposed solution involves a smart pill device that, once activated by the acidic stomach juices, collects a bacteria-containing gastric aspirate sample before sealing itself off and continuing through the GI tract for collection upon excretion. Once it has been collected, the gastric acid sample may be used with the GeneXpertTM machine for diagnosis. Bench testing has demonstrated that this device is able to collect an equivalent sample to gastric lavage per administration (5 mL), before stomach emptying occurs (6 minutes), and is applicable in South African children due to its FDA-approved size (11x26 mm), the incorporated delivery lubricant, and its low cost (8.00 USD per pill). We expect the implementation of this device to revolutionize TB diagnosis in the South African pediatric population due to its simplistic and naturally intuitive design.
A Novel Screening Device for Detection of Early Stage Ovarian Cancer
Julia Fraseur, Amanda Goetze, Stephanie Klunk, Ivan Nantung
Ovarian cancer will claim the lives of over ten thousand women in the United States this year. When found in earlier stages, such as stage one, the five-year survival rate is 92%. However, when ovarian cancer is diagnosed in stage four, the latest stage of progression, patients have only a 17% survival rate. Due to being asymptomatic, the vast majority of ovarian cancer cases are caught in late stages once the cancer has metastasized in multiple organs or tissues. This illustrates the need for an effective screening technology that can detect early stage ovarian cancer. Circulating tumor cells (CTCs) are known to be present in the blood stream in early stages of ovarian cancer. However, these CTCs exist at extremely low concentrations and cannot be found using standard blood screening methods.
This project’s solution is a device that improves CTC detection technology through collection of magnetic beads that are bound to CTCs in a 20 mL blood sample. The device features an optimized flow chamber that creates laminar flow for efficient processing that maximizes detection in samples with trace amounts of CTCs. The design allows for processing of larger samples of blood, which is a necessity in using this test as a screening method, as it improves sensitivity. This feature, along with being ovarian cancer specific, makes it unique from current screening methods used in oncology. Implementing this device as a universal screening tool will provide clinicians an opportunity to detect ovarian cancer in an early stage. When ovarian cancer is detected early, a broader range of treatment options emerge that are more effective and less expensive than end stage care. The financial and health benefits of this device will create a more promising future for women and families affected by ovarian cancer.
Improving Hemodynamic Monitoring and Temperature Control during Anesthesia
Stephanie Eichman, Ryan Byer, Cassie Parker, Tori Clift, Robert Wujek, Sahil Sanghani
Every year, 40 million North Americans undergo procedures requiring general anesthesia. As many as 50 - 90% of patients experience problems during these procedures including difficulty controlling body temperature as well as inaccurate monitoring of blood oxygenation which causes suboptimal anesthesia. Perioperative hypothermia and inaccurate anesthesia administration cause complications that increase recovery time, which incurs extra cost to the patient and the healthcare system. This device will lower costs and improve patient outcomes for patients undergoing general anesthesia.
This design integrates reflective pulse oximetry technology into an esophageal tube specially molded to allow for the flow of a heated fluid through the device, encouraging heat transfer to take place. The flow rate of fluid through the device is controlled by a pump which also controls the temperature of the fluid. The tube utilizes the esophageal environment to access highly vascularized tissue for more accurate hemodynamic monitoring and internal heat exchange. This device is the first to provide accurate real time blood oxygenation levels for both hemodynamically stable and unstable patients as well as provide patient core body temperature control.
Studies show that esophageal pulse oximetry produces more accurate results than external monitoring methods. Also, through bench and animal testing the proof of concept of the combination technology has been validated. Within a one to three hour time span, the device provides higher temperature stability than external warming methods and reliable oxygenation readings for more accurate patient monitoring. The novelty of this product lies within the integration of two methods as no one has ever done this before. There is also potential for more sensors to be integrated into the esophageal tube to provide more patient metrics to hospital personnel. This increased functionality will benefit more patients than either of the technologies can serve by themselves.
Traumatech: Brain Injury Detection
Alyse Marie Allred; Andrew Houvenagle; Alan Poon; Alex Sommer; Richmond Toy; Davis Wagner
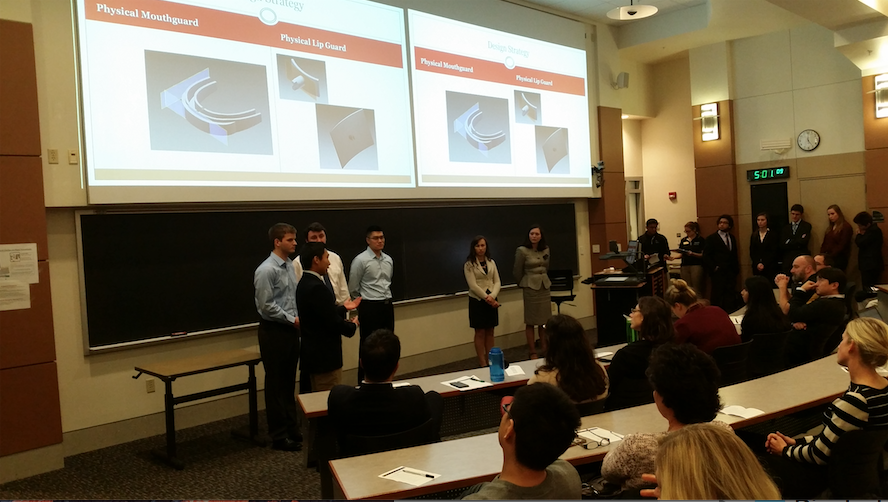 Traumatic brain injuries (TBI’s) occur in approximately 1.7 million Americans each year, often in an athletic setting. The cost of treating traumatic brain injuries totals billions of dollars each year. Although a TBI is able to heal properly if given enough time, the occurrence of a second TBI before the first has properly healed has a 50% chance of resulting in death. Often athletes do not realize, or are not willing to admit, that they have suffered a TBI (such as a concussion). This lack of notification results in approximately 40% of players returning to play too soon. Due to this problem, there needs to be a method that can measure the forces applied to the head that is accurate and can determine whether or not the user is suffering from a TBI. Traumatech has designed a mouthguard capable of recording and analyzing forces applied to the head. The forces recorded are accurate to within 15%. Over the course of this project, Traumatech has successfully integrated an electronic component into a mouthguard that accurately reads force and directional impacts on the head. From there, it can upload this information to a computer application that analyzes the data for potential concussions and displays this information in an easy to use graphical user interface. The end goal of this device is to reduce the number of
Traumatic brain injuries (TBI’s) occur in approximately 1.7 million Americans each year, often in an athletic setting. The cost of treating traumatic brain injuries totals billions of dollars each year. Although a TBI is able to heal properly if given enough time, the occurrence of a second TBI before the first has properly healed has a 50% chance of resulting in death. Often athletes do not realize, or are not willing to admit, that they have suffered a TBI (such as a concussion). This lack of notification results in approximately 40% of players returning to play too soon. Due to this problem, there needs to be a method that can measure the forces applied to the head that is accurate and can determine whether or not the user is suffering from a TBI. Traumatech has designed a mouthguard capable of recording and analyzing forces applied to the head. The forces recorded are accurate to within 15%. Over the course of this project, Traumatech has successfully integrated an electronic component into a mouthguard that accurately reads force and directional impacts on the head. From there, it can upload this information to a computer application that analyzes the data for potential concussions and displays this information in an easy to use graphical user interface. The end goal of this device is to reduce the number of
serious injuries due to secondary concussions, and enable coaches and athletic advisors to make more sound decisions regarding the removal of players from games. Eventually, it is anticipated that this or similar devices become standard in athletics across the country.
