International partnerships to tackle global health issues
Purdue biomedical engineering researchers are focused on addressing challenging global issues, while benefiting through collaborations with interdisciplinary colleagues who assist in meeting needs that exist in developed and developing regions.
International research efforts led by our faculty include: portable devices to identify pathogens, a digital cancer diagnostic tool, using silk for its medical and optical properties, low-cost stents for esophageal cancer patients, and a platform to detect doctored images on the internet.
- Point-of-care disease detection in at-risk regions: Jacqueline Linnes and Tamara Kinzer-Ursem, both assistant professors in biomedical engineering, are working on a low-cost portable device to detect the presence of a pathogen within 30 minutes. Already partnering with a group in Haiti, the researchers say the device puts the power of a lab in the palm of a hand and could significantly improve global health.
- Development of a cancer predictive model: Building on the successes of an international Digital Human for Drug Development (DHD2) collaboration with scientists at the Korea Institute of Science and Technology (KIST) and others, Kinam Park, Showalter Distinguished Professor of Bioengineering and professor of pharmaceutics, and his team from Purdue are leading an effort to develop a multiscale computer model of human physiology for screening and identifying effective and safe drug candidates for treating cancers and other diseases.
- Leveraging silk for its therapeutic properties: Young Kim, associate professor of biomedical engineering, and his team are partnering with South Korean researchers to investigate the use of silk-based flexible and wearable fabrics and nanomaterials for their unique bio-sensing and therapeutic properties as well as optical and self-cooling benefits.
- Improving testing for anemia in resource-limited settings: Young Kim and an interdisciplinary research team are equipping smartphones with a program to analyze blood hemoglobin content for levels of anemia.
- Designing low-cost stents for esophageal cancer patients: Andrew Brightman, assistant head of biomedical engineering and associate professor of engineering practice, is leading a team that is partnering with IU School of Medicine and Moi Teaching and Referral Hospital in Kenya to design low-cost stents to relieve suffering of advanced-stage esophageal cancer patients in Kenya.
- Detecting doctored images and video: Ed Delp, a professor in the Weldon School and the Charles William Harrison Distinguished Professor of Electrical and Computer Engineering, is a lead researcher on a global media forensics initiative to help U.S. intelligence analysts detect doctored images by developing a platform for scanning millions of images and videos posted online each day. The team hopes to leverage machine learning along with image and signal-processing techniques to help spot images that might have been falsified.
Point-of-care disease detection in at-risk regions
Tamara Kinzer-Ursem and Jacqueline Linnes are developing a point-of-care disease detection device, called PathVis, which aims to deliver results in 30 minutes or less, particularly useful in countries where early detection is vital.
The researchers are planning to travel to Gressier, Haiti, next spring to conduct field tests for cholera in collaboration with the University of Florida’s Emerging Pathogens Institute Institute as part of the platform device to detect multiple diseases.
“Global aid organizations have told us that they need a fast, low-cost, portable and accurate diagnostic device to fight these diseases,” Kinzer-Ursem says. “Cholera, HIV, malaria and dengue are all prevalent but preventable pathogens. We are on a mission to take these powerful devices that you carry around every day and turn them into laboratories to detect disease.”
Joining Kinzer-Ursem and Linnes on the project are Steven Wereley, a professor in the School of Mechanical Engineering, and Katherine Clayton, a graduate student researcher in the School of Mechanical Engineering.
The Purdue team’s research won first place in the annual Wireless Innovation Project, with the project receiving a $300,000 grant ($100,000 a year for three years) from the Vodafone Americas Foundation. The award, announced in June at the 2017 Social Innovation Summit in Chicago, is the latest of many awards the project has received in the past six months.
Existing technology is categorized in two ways: first, a fluorescence technology that is accurate, but expensive to make and to use; second, a rapid diagnostic device based on flow strip technology, which is similar to an inexpensive pregnancy test but is not very accurate because a lot of the pathogen or antigen must be present to yield a positive diagnosis.
With PathVis, a sample is placed in a test cartridge with disease-specific reagents and some small beads. The test cartridge is then placed under a smartphone camera. If a pathogen is present, a chemical reaction increases the viscosity of the solution and hinders the movement of the beads. If a pathogen is not present, the solution maintains a low viscosity, and the beads move easily. The particle motion is measured and analyzed via proprietary algorithms in a smartphone application.
From sample collection to test result, the entire process takes about 30 minutes. Algorithms in the smartphone app use the Global Positioning System to geotag and time-stamp data and upload it to the cloud. This enables aid organizations and governments to monitor the detection of disease in real time and take quick take action as needed to deliver clean water and initiate a public health campaign.
“The exciting part of this is the broad application space that this fundamental technology has,” Kinzer-Ursem says. “We are also detecting different diseases such as malaria and HIV. The platform can be readily adapted to other important pathogens in the future.”
Development of cancer predictive model
An interdisciplinary team of Purdue engineers, pharmacists and veterinarians is working to establish a predictive framework for rapidly screening and identifying effective and safe drug candidates and their delivery systems for treating cancers and other diseases.
This effort focuses on developing computational modules, including pharmacokinetics and biodistribution of drug delivery systems, spatiotemporal distribution of drugs at major organs and tumors, transmembrane transport and intracellular distribution, and cellular signaling pathways and pharmacodynamics of drug molecules.
The project is an extension of Purdue’s global efforts behind the ambitious Digital Human for Drug Development (DHD2) project, a collaboration between Purdue researchers and the Korean Institute of Science and Technology (KIST).
“Before, our Purdue team had expertise in blood circulation and diffusion. We now are introducing the immune response aspect,” Kinam Park says. “That’s a big deal today because many new cancer treatments are based on immune response. That’s where we have this new expertise, which will make our entire approach stronger.”
Joining Park on the project are Elsje Pienaar and Tamara Kinzer-Ursem, both assistant professors of biomedical engineering, Bumsoo Han, professor of biomedical and mechanical engineering, and David Umulis, associate professor of biomedical, biological, and agricultural engineering, as well as Tony Lei Li, Allen Chao Chair and Professor of Industrial and Physical Pharmacy, and Debbie Knapp, the Dolores L. McCall Professor of Comparative Oncology.
These researchers say their efforts will be done in parallel with and validated by experimental animal tumor studies. At the same time, testing will focus on the efficacy and toxicity of new drug candidates a priori. The model, they say, also will lay the groundwork for predictively screening a broad spectrum of new chemical entities and delivery systems for various diseases in silico, which uses computer modeling to examine the pharmacologic or physiologic process.
“The goal is to develop molecular, cellular and tissue level simulations, with specific cancer phenotypes and then linking those scales via multiscale modeling,” Umulis says. “We are also studying how the immune cells function in different regions to combat cancer.”
The proposed model for the project relies on Model-Based Design of Experiments (MB-DOE) methods more commonly used in engineering design but until now have not been widely used in life sciences research and development, Pienaar says.
“This team is integrating multiple types of data into one coherent system so that what we learn from the lab in in vitro and clinical studies can help close the gaps that currently exist, and in so doing, predict outcomes in model systems and humans,” says Umulis, who is leading a short course in Guangzhou in China in November (for the third time) that focuses on modern practices in systems biology and data integration.
Launched in 2014, Purdue’s DHD2 project is aimed at changing the way drugs are developed around the world — rendering the process speedier, cheaper, safer and more effective and accelerating the evolution of personalized medicine. The DHD2 project has been funded by KIST and the Weldon School of Biomedical Engineering.
Park’s research has focused on the use of various polymers and hydrogels for controlled drug delivery, and his current research concentrates on mechanistic understanding of long-acting depot formulations, in particular biodegradable PLGA polymers. In addition, Park also is working on the development of new environment-sensitive polymers with researchers at Kazakh National University in Almaty, Kazakhstan.
Leveraging silk for its therapeutic properties
Throughout history, silk has clothed royalty and the elite, evolving with fashion trends as one of the most coveted fabrics of all times. Today, Young Kim and his international research team see native silk for its therapeutic and bio-sensing benefits — as a disinfectant or wearable bandage or garment.
In collaboration with the U.S. Air Force Research Laboratory-Wright-Patterson Air Force Base, Kim’s research group also is studying silk’s light-scattering properties for use in optics and for the natural material’s self-cooling effects — in hope of using silk as a material in a temperature-controlled tent that doesn’t rely on electricity.
“Silk is a really nice bio-polymer and it’s biocompatible, so it’s safe to wear or to be used in implantable devices,” says Kim, who also serves as director of Purdue’s Natural and Biological Photonics Laboratory. “Our results will provide the groundwork for exploiting natural silk as a photonic nanomaterial hybridization platform to implement embedded functionalities in a fiber geometry, which can be constructed into large-area and continuous fabrics.”
Joining Kim on the project are Seong-Ryul Kim, a visiting researcher from the National Institute of Agricultural Sciences, Rural Development Administration in South Korea; and postdocs Jung Woo Leem and Seung Ho Choi.
An exciting application of the silk research is a photo-inducible, genetically encoded approach for killing harmful pathogens. Fluorescent silk, which is produced by silkworm transgenesis of fluorescent proteins, can potentially inactivate harmful viruses and bacteria when used in wearable garments such as masks and gloves.
“The silk acts more like a host material. And because of this transgenic cell, the fluorescent protein is fully expressed embedded in the silk fiber, so it’s a single entity,” Kim says. “When the silk is exposed through a green light, for example — we don’t have to use any harmful UV illumination — it generates radicals that inactivate some of the harmful pathogens.”
Kim also is examining the unique combination of transgenic silk and facile metal nanoparticle hybridization, which offers nontoxic fluorescent media while utilizing plasmonics for enhanced photoluminescence. This particular hybridization is inspired by a common method in the 19th century of adding metal — in Kim’s case, silver — to the thread to increase the weight of silk fabrics and raise its sale price.
Because of its strong affinity to metal ions, the natural material can be enhanced with plant-derived polyphenolic chemistry to form nanoparticulated metal with finite sizes inside the interfibrillar nanostructures of silk. “And within this structure, we can basically insert some small metal nanoparticles that generate hot spots to enhance the fluorescent signal,” he says. This would open the door for silk’s use in lasers, optics, fiber optics, thermal photonic devices, and even quantum information processing.
Kim has received a $110,000 grant from the U.S. Air Force Office of Scientific Research and a $150,000 grant from the South Korea Rural Development Administration to advance his research. The project also has funding from the Rural Development Administration’s Cooperative Research Program in South Korea. His team’s research was recently published in Materials Horizons, which is a new premier journal of Royal Society of Chemistry: http://pubs.rsc.org/en/content/articlelanding/2017/mh/c6mh00423g#!divAbstract
Photo (top right): Young Kim, left, and postdoc researcher Seung Ho Choi examine a silk pod in the Natural and Biological Photonics Laboratory at the Martin Jischke Hall of Biomedical Engineering. Through a partnership with South Korean partners, Kim and his team are researching natural silk for its therapeutic and bio-sensing benefits. (Purdue University photo/Phillip Fiorini)
Photo (bottom right): A look at a silk pod in Young Kim’s laboratory. (Purdue University photo/Phillip Fiorini)
Improving testing for anemia in resource-limited settings
 The National Institutes of Health Fogarty International Center has awarded Young Kim and Md Munirul Haque, research scientist with the Regenstrief Center for Healthcare Engineering and their interdisciplinary research team, a $385,000, two-year grant to improve mobile testing for anemia in resource-limited settings. The researchers will investigate the possibility of equipping mobile smartphones with a program to analyze blood hemoglobin content for levels of anemia and to measure those levels with the accuracy of conventional blood tests.
The National Institutes of Health Fogarty International Center has awarded Young Kim and Md Munirul Haque, research scientist with the Regenstrief Center for Healthcare Engineering and their interdisciplinary research team, a $385,000, two-year grant to improve mobile testing for anemia in resource-limited settings. The researchers will investigate the possibility of equipping mobile smartphones with a program to analyze blood hemoglobin content for levels of anemia and to measure those levels with the accuracy of conventional blood tests.
Anemia is a global public health problem, affecting more than 2 billion people worldwide, including 50 percent of pregnant women and 69 percent of preschool children in Kenya, East Africa, where development and testing of smartphone-based bloodless spectrometerless Hemoglobin Analyzer technology — will be aided by AMPATH, the Academic Model Providing Access to Healthcare. AMPATH is a consortium of academic health institutions, including Purdue and the Indiana University School of Medicine, that have joined together to partner with Kenya-based Moi Hospital and University to tackle the challenges of disease and poverty.
This study combines medical device development, clinical laboratory testing, computer science, and cultural sensitivity,” said Kim. “Partnering with AMPATH allows us to reach a severely affected population in order to fine-tune and make reliable, portable anemia testing an option for Kenya.
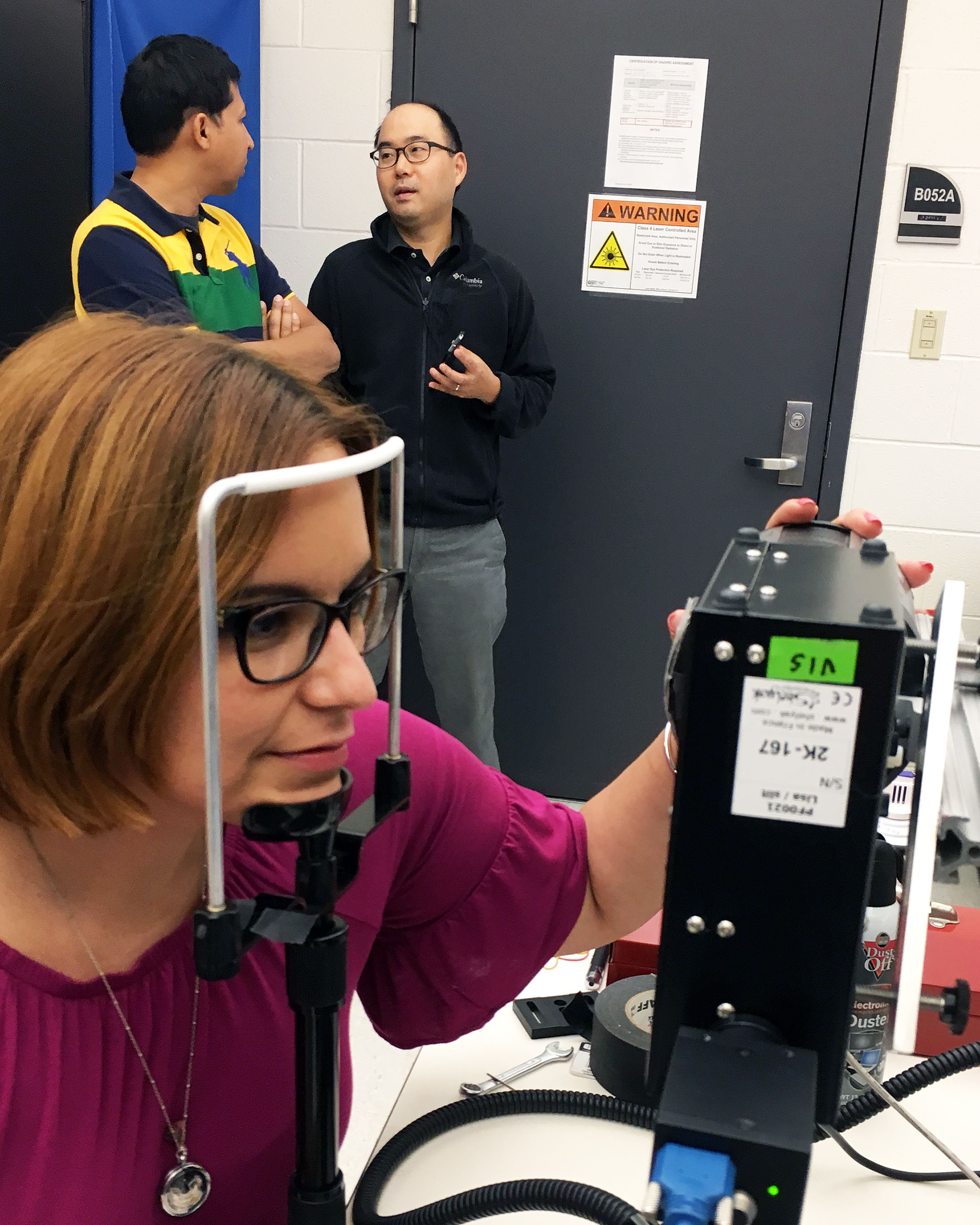
Photo (right): Graduate student Michelle Visbal Onufrak works with a dual port hyperspectral imaging system as professors Young Kim and Md Muniral Haque converse in the background.
Design of a low-cost stents for esophageal cancer patients in Kenya
Kenya has one of the highest incidences of esophageal cancer, a common but devastating disease in the developing world. Physicians at Moi Teaching and Referral Hospital (MTRH) in western Kenya regularly see patients with esophageal cancer. But, by the time most of these patients arrive at MTRH, the cancer is very often in an advanced state and the patient is eligible for only palliative end-of-life care, which involves using stents to restore the opening of the esophagus.
Unfortunately, the current clinical options are rigid plastic tubing or Self-Expanding Esophageal Metal Stents (SEMS). Rigid plastic tubing is risky and inefficient since migration is typical, multiple sizes and multiple deliveries are typically needed, and each deployment further damages esophageal tissue. SEMS are significantly safer, but much more expensive. The price of the least expensive SEMS is between $100 and $150—well beyond the resources of many Kenyans. This forces patients to choose between cost and risk of serious complications. Many Kenyan families choose to deplete their entire savings to provide this relief.
“A low-cost option to restoring the opening of the esophagus and improving the quality-of-life for these terminal patients is critically needed,” says Dr. Tom Carr, assistant professor of clinical medicine, Indiana University School of Medicine, and North American Director (Gastroenterology) AMAPATH Consortium.
Brightman is leading a multidisciplinary team of collaborators from around the world to find a solution. In addition to Thomas Carr, MD, the team includes: Lester Smith, PhD, assistant research professor, Department of Radiology & Imaging Sciences, Indiana University School of Medicine; John Githaiga, associate professor, director of Innovations Firm, School of Engineering at Moi University; and Fatuma Some, MBChB, MBA, MD (Gastroenterology) at MTRH.
“Our plan is to design and develop an esophageal stent that will not only relieve the suffering caused by esophageal cancer, but it can be made in Kenya and will be affordable for all Kenyans,” says Brightman.
The team is currently working with students in the Weldon School of Biomedical Engineering to co-design and fabricate two initial prototypes for the low-cost esophageal stenting with preclinical testing beginning this Fall. They plan to take the best of these prototypes back to Kenya in May 2018 for evaluation and feedback from the physicians at MTRH.
Detecting doctored images and videos
Ed Delp is part of an international research effort to develop a system for the military that would detect doctored images and video and determine specifically how they were manipulated. The research involves the University of Notre Dame, New York University, University of Southern California, University of Siena in Italy, Politecnico di Milano in Italy, and University of Campinas, in Brazil.
“It's a very ambitious program,” says Delp, the team's principal investigator and director of Purdue's Video and Image Processing Laboratory, or VIPER Lab. “We have plenty of work to do in four years. One of the things we are doing is bringing to bear a lot of important tools from signal and image processing, computer vision and machine learning.”
A huge volume of images and video of potential intelligence value are uploaded daily to the internet. Visual media, however, are easily manipulated using software tools that are readily available to the public. As part of a four-year, $4.4 million project funded by the Defense Advanced Research Projects Agency, Delp and his partners hope to leverage machine learning along with image and signal-processing techniques to help spot images that might have been falsified.
“Now there is an unfair advantage to the manipulator,” says Delp. “It’s similar to an arms race in the sense that as better algorithms are able to detect doctored media, people are able to change how they do the manipulation. Many open-source images and videos are of potential use to the intelligence community, but how do you know those images can be trusted?”
The researchers will strive to create an “end-to-end” system capable of handling the massive volume of media uploaded regularly to the Internet. The system will require specialized machine-learning computers and will be designed to automatically perform processes needed to verify authenticity for millions of videos and images.
“Many tools currently available cannot be used for the tens of millions of images that are out there on the internet,” Delp says. “They take too long to run and just don’t scale up to this huge volume. I think the biggest challenge is going to be the scalability, to go from a sort of theoretical academic tool to something that can actually be used.”
