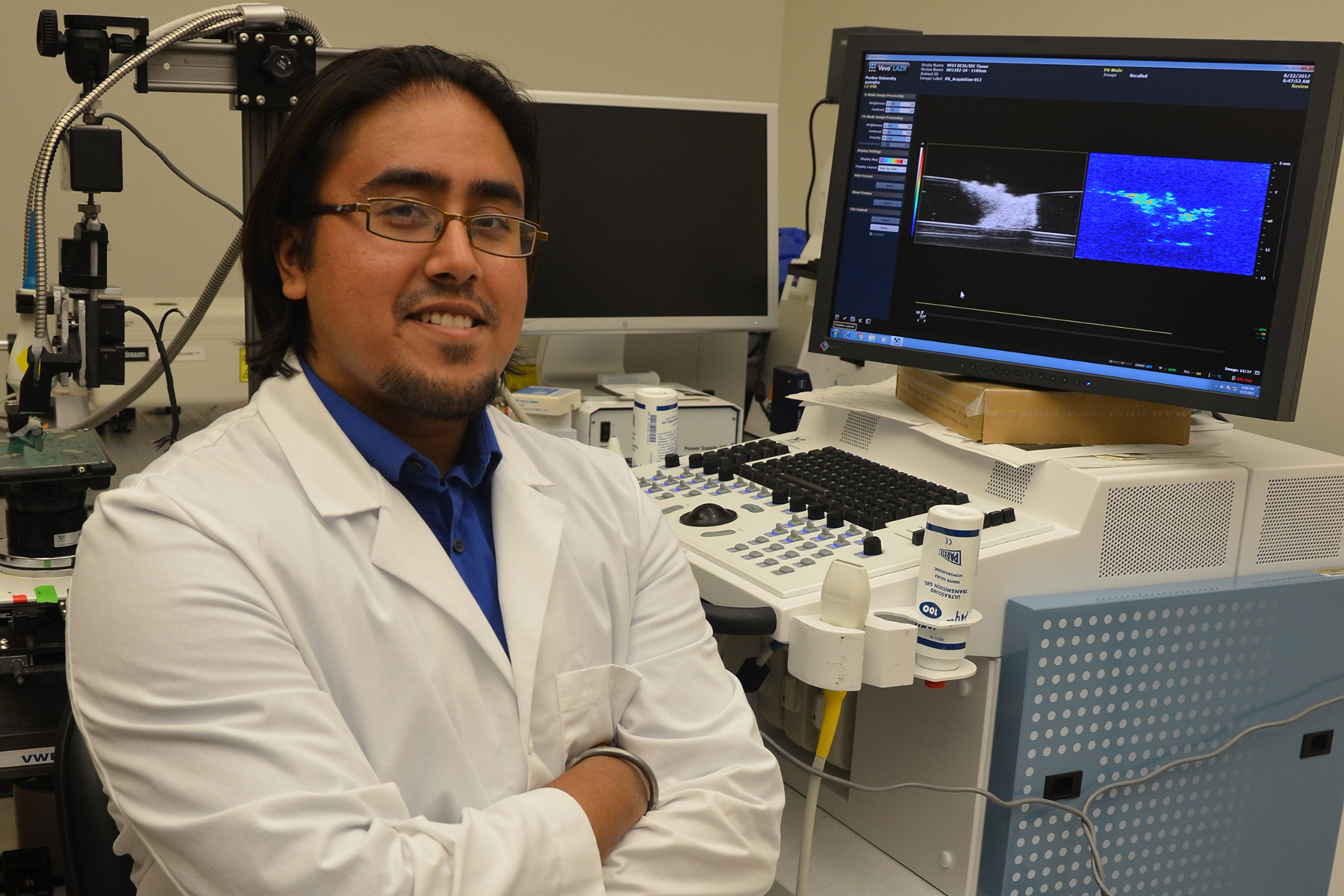
Sangha receives Baxter Young Investigator Award
 “My overarching goal is to develop devices and methods that will one day positively impact both physicians and patients,” Sangha said. “Receiving this recognition from Baxter, a company whose mission is to provide cost-effective, high quality, and innovative healthcare products to the world, gives me faith that I am on the right path to accomplishing my goal.”
“My overarching goal is to develop devices and methods that will one day positively impact both physicians and patients,” Sangha said. “Receiving this recognition from Baxter, a company whose mission is to provide cost-effective, high quality, and innovative healthcare products to the world, gives me faith that I am on the right path to accomplishing my goal.”
Sangha’s project is titled, “Vibrational Photoacoustic Tomography: Applications for Intraoperative Surgical Imaging.” Vibrational Photoacoustic Tomography (VPAT) is an imaging technique that uses near-infrared light to induce acoustic waves, which can be used to recreate images of tissue in more detail than conventional clinical imaging techniques. When used with ultrasound, clinicians receive both structural and compositional information about the tissue, which can potentially aid in the diagnosis and treatment of various diseases.
Sangha’s work is focused on optimizing the technique to improve depth of penetration and image quality, as well as developing VPAT for various applications, including detecting cancerous cells around the edges of breast tumors and imaging destroyed cardiac tissue.
Current methods for breast tumor margin detection are invasive, time-consuming, and typically result in a reoperative rate of up to 39 percent. Sangha is exploring the use of VPAT, ultrasound, and inverted Selective Plane Illumination Microscopy (iSPIM) to assess breast tumor margins in human breast biopsies. The goal of the study is to assess the performance of the VPAT system to correctly characterize tumor margins in both a single-modality and multi-modality approach.
Cardiac arrhythmia treatment requires the use of a radiofrequency catheter to ablate or destroy a small area of dysfunctional cardiac tissue. The limitation of this approach is that clinicians have difficulty determining the volume of tissue burned during the surgical procedure, especially for advanced arrhythmia that require multiple burned lesions. Preliminary data from Sangha’s study have shown that VPAT coupled with ultrasound can potentially enable clinicians to assess the volume and severity of ablated cardiac tissue during surgery.
Baxter sponsors this annual award program to celebrate and promote innovative research that has relevance to the company’s portfolio and is conducted by graduate students and postdoctoral fellows. Sangha’s award included a $500 cash prize.
