Research
Ongoing Projects: Distributed Point of Care (POC) Molecular Diagnostics
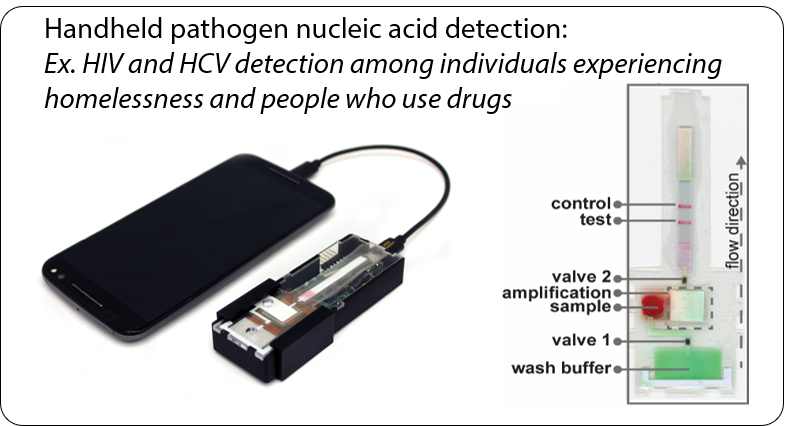
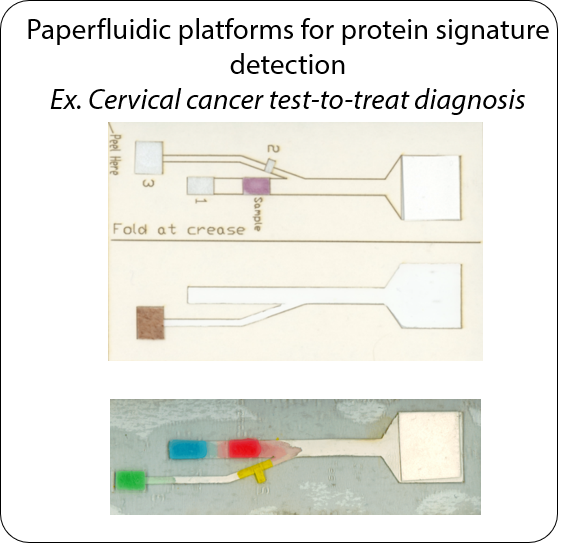
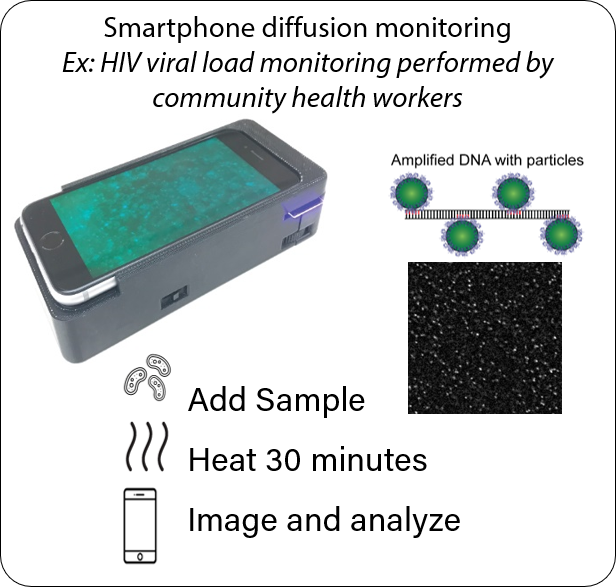
The future of point of care testing enables general practitioners and patients themselves to detect diseases. However, these distributed sample-in answer-out tests will require simple operation, interpretation, and connectivity to other healthcare resources. Working with our clinical, commercial, and public health collaborators to translate technologies out of the lab and into the field, we create microfluidic biosensors that efficiently diagnose a variety of environmental, bacterial, and viral pathogens at the point of care. This research is creating rapid diagnostics and devices that enable disease prevention and improved care anywhere in the world. The applications of our work range from global health to biodefense to personalized medicine.
Biosensor design and Device Development
The majority of the research in the Linnes Lab focuses on using state of the art microfluidic and paperfluidic technologies to prevent, detect, and better understand the pathogenesis of these infectious diseases. In particular, these include developing point of care diagnostics for rapid disease detection, and determining the efficacy of therapeutic interventions via miniature bioassays for low resource settings. We are utilizing a range of innovations from paper-based fluidic connections, miniaturized low-power heating, and smartphone optics to develop portable, instrument-free, molecular diagnostics that are as easy to use as a digital pregnancy test. These days our research involves both developing new assays and scaling up our existing platforms.
Funding
-
Gordon and Betty Moore Foundation (Moore Inventor Foundation funding for paperfluidic platform development)
- NIH National Insitute of Allergy and Infectious Diseases (R61/R33 funding for HIV viral load monitoring)
- NIH National Institute on Drug Abuse (DP2 funding for Acute HIV and HCV detection)
- NIH National Cancer Institute (R01 funding for Cervical cancer detection)
- NSF Division of Industrial Innovation and Partnerships
- Bill and Melinda Gates Foundation, Grand Challenges Explorations (HIV detection)
- Purdue Shah Family Laboratory for Global Innovation Lab (HIV, Cholera water contamination, Cervical cancer screening)
- Purdue Institute for Immunology, Inflammation, and Infectious Disease (Whooping cough detection)
Human Centered Design
We co-design and evaluate our diagnostic technologies in collaboration with with community health workers, providers, and patients in order to ensure that our diagnostic devices fit their specific use cases and needs. In collaboration with experts in both public health and engineering education, we are developing and formalizing frameworks for empathic and equitable design from needs-finding to usability testing in order to improve medical device and biosensor translation, implementation, and adoption.
Funding
- Gordon and Betty Moore Foundation (Moore Inventor Foundation funding for paperfluidic platform development)
- NIH National Insitute on Mental Health (R61/R33 funding for HIV viral load monitoring)
- NIH National Institute on Drug Abuse (DP2 funding for Acute HIV and HCV detection)
- NIH National Cancer Institute (R01 funding for Cervical cancer detection)
- NSF Div Of Engineering Education and Centers (Empathy in Design)
Past Projects
Wearable Devices for Substance Use Monitoring and Overdose Detection
To combat the ongoing Opioid Epidemic and improve medication adherence, we have designed unobtrusive devices that help patients to overcome their addictions. We explored temporary tattoo-based biosensors to non-invasively measure drug concentrations from sweat and wearable smartwatches to measure physiologic responses to overdose ranging from changes in heartrate, SpO2 and Respiration. Wearable vital signs detection technology is being commercialized by Rescue Biomedical LLC (co-founded by Dr. Linnes)
Funding
- Ralph W. and Grace M. Showalter Research Trust
-
NIH National Institute of Drug Abuse
-
Purdue Institute for Integrative Neuroscience
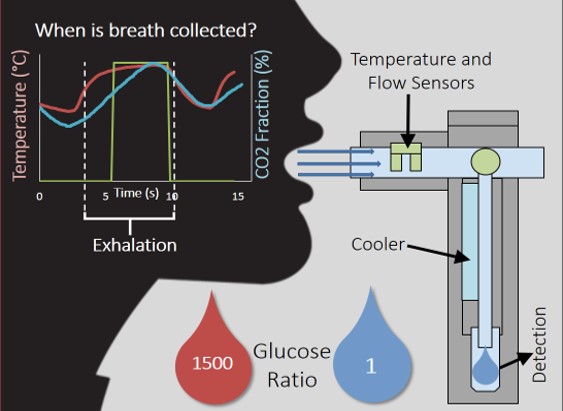
Non-invasive glucose measurement
Two thirds of patients with diabetes avoid regularly monitoring their blood glucose levels because of the painful and invasive nature of current blood glucose detection. As an alternative to blood sample collection, exhaled breath condensate (EBC) has emerged as a promising non-invasive sample from which to monitor glucose levels. We explored methods to standardize thet collection of EBC and developed biosensors to detect the minute concentrations of glucose and other analytes in this complex sample matrix.
Funding
- Indiana CTSI
- NIH National Institute of Biomedical Imaging and Bioengineering