Collaborations breed success
Collaborations breed success
| Author: | Della Pacheco |
|---|---|
| Magazine Section: | Our People, Our Culture |
| College or School: | CoE |
| Article Type: | Issue Feature |
| Page CSS: | .sidebar.right {
top: -1200px; } |
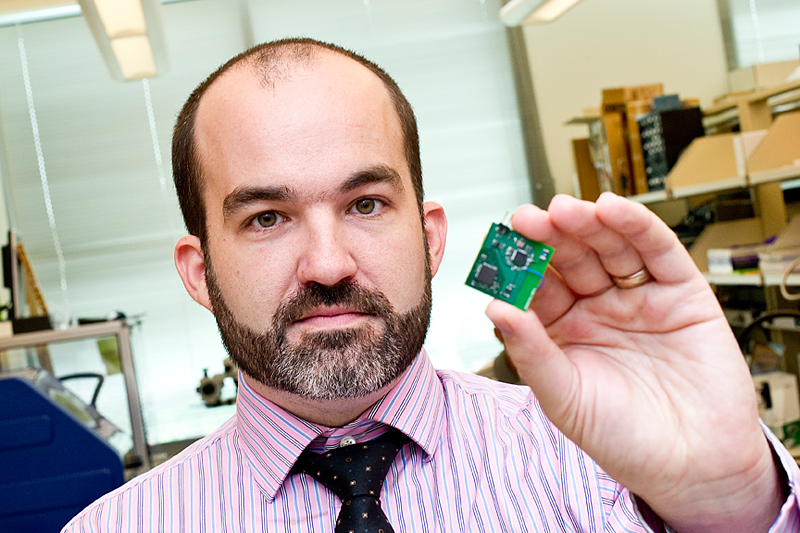
| Feature Intro: | Center for Implantable Devices faculty researchers team with clinicians and commercial partners to solve medical puzzles. |
Imagine moving a robotic limb with your thoughts. Stopping an epileptic seizure before it begins. Sensing subtle pressure changes in the eye to prevent blindness.
Purdue biomedical engineering faculty not only imagine this future but are developing implantable medical devices to make it happen.
Pedro Irazoqui, associate professor of biomedical engineering and director of the Center for Implantable Devices at the Weldon School of Biomedical Engineering, says the mission of the center, which recently marked its first anniversary, is to lead the research, development, and translation of implantable medical devices; formalize collaborations between faculty, clinicians and commercial partners; and to maximize clinical impact.
“We want to see our work end up in humans to improve quality of life and address real medical needs,” Irazoqui says. “Its not just being collaborative between physicians and engineers but it’s also bringing in the corporate element as well.”
Biomedical faculty work with clinicians to identify needs and find a corporate sponsor who is interested in taking the proposed solution to market. Earning a combination of corporate, foundation and federal grant funding helps finance work from the conceptual stage to a point where it can be sent to a commercial partner for commercialization.
Houston-based Cyberonics Inc. contributed $2 million for epilepsy research. Epilepsy research constitutes about half of the center’s work.
Jenna Rickus, associate professor of agricultural and biological engineering and biomedical engineering, is developing a new type of biosensor that will measure the presence or absence of different neurotransmitters in the brain in order to sense when an epileptic seizure is about to begin.
One of the challenges of implantable devices is encapsulation that may occur when the body senses a foreign object.
“We think that we can overcome this by using wires so thin that the body doesn’t recognize them as foreign objects,” Irazoqui says. “We would use magnetic fields to position these flexible wires inside the brain.”
The team is also developing algorithms that will process activity to detect when a seizure is about to begin. In work with Dr. Robert Worth, professor of neurosurgery and a respected neurosurgeon at the Indiana University School of Medicine, the device has shown promise in animal trials.
Eugenio Culurciello, associate professor of biomedical engineering, has done extensive research in optical sensing. Researchers have tried to record brain activity electrically but electrodes degrade in performance over time. Culurciello is working to develop an optical sensor — a computer chip — that can detect light emitted by voltage-sensitive dies in the brain. This is a less invasive procedure with lower risk of infection and might be a quicker and more accurate way of monitoring neural activity.
Irazoqui is quick to point out that he did not start the center but it was born out of a natural collaboration among Purdue engineering faculty.
He came to Purdue to work on implantable devices but their production requires a complete package, including circuitry, wireless communications and animal work.
“One of the great things about Purdue is that in almost anything you want to do there is an expert already here,” he says. “When I was looking at wireless, someone suggested Professor William Chappell in electrical engineering. In addition to his work in that arena, he is also an expert in packaging.”
Irazoqui sought out Kaushik Roy, the Roscoe H. George Professor of Electrical and Computer Engineering, who is known globally for his work with digital circuit design.
Kevin Otto, assistant professor of biological sciences and biomedical engineering, is known for his work with the interface between implantable devices and biology.
“At the time the center started, my intent was to not bring anyone into the center unless there was a real connection,” Irazoqui says. “In every case I wanted to be able to say exactly what that person brings to the center.”
Addressing real medical needs
Working with Dr. Todd Kuiken, director of the Rehabilitation Institute of Chicago, and with support from the Defense Advanced Research Projects Agency or DARPA, the team is developing a device to enable Kuiken’s targeted muscle reinnervation procedure to help amputees coming back from the wars in Afghanistan and Iraq. DARPA is part of the Department of Defense.
Researchers have been trying for decades to implant a device in the brain to allow amputees to move robotic arms by brain activity. Kuiken is taking a different approach.
“Recording electrical activity from the brain is very tricky,” Irazoqui says. “If you lose an arm, the nerve that used to travel down the arm is still there as are the pectoral and lateral muscles. What Dr. Kuiken does is reroute the nerve to connect with unused muscles that used to move the missing limb. He then records the muscle contraction and uses that to control the prosthetic arm. We provide the implantable wireless electrodes to enable his work.”
Current studies use electrodes attached to the skin to record muscle activity but they easily fall off due to sweating and movement. When this happens, the entire process must be reprogrammed and recalibrated.
Through the center’s work, researchers want to develop and implant dozens of electrodes no larger than a grain of rice into the muscle to record activity and to transmit information wirelessly. Even if the tiny electrodes become encapsulated, the amplitude of muscle signals is so large that they can still be recorded. In late July the center received a $2.5 million grant from DARPA to support the research.
Another area of research is related to glaucoma, a disease that causes blindness in millions of people worldwide. There are numerous treatments to slow the condition but none are totally effective and all have significant side effects. Currently, a continuous monitoring device is not available, but its development may open up new avenues for treatment.
A small implantable device will be very beneficial for glaucoma and the center is collaborating with Dr. Simon John of the Howard Hughes Medical Institute at the Jackson Laboratory to develop such an instrument.
“Professor John approached me several years ago and asked if we could develop a device so small that it could fit inside the eye of a mouse and could monitor pressure continuously to track glaucoma,” Irazoqui says. Mice, it seems, are much better models for what happens in human glaucoma than nearly any other animal except primates.”
The collaboration to develop a mouse-sized device has flourished. It is funded through a $4 million Howard Hughes Medical Institute Collaborative Innovation Award to John, Irazoqui and Chappell. An advantage of developing mouse-implantable devices is that they can be applied to any larger species. SOLX Inc., a startup company based in Boston, intends to license this miniature technology to use in human patients. SOLX recently raised $20.5 million from life science venture capitalists, a portion of which is designated to bring glaucoma devices into human clinical trials.
Regulatory challenges
The researchers hope to move from concept to human clinical trials, but regulatory challenges can be overwhelming.
“For the targeted muscle reinnervation project, we would like to see it go into humans in three years,” Irazoqui says. “Being wildly optimistic, we need to finish the device this year, spend next year working with a company to make a product from our prototype, and then spend a year going through FDA approval.”
If all of that happened, the next step is obtaining an IDE — an investigational device exemption from the FDA. Once that is in hand, a limited number of devices can be implanted in patients. Next is receiving Institutional Review Board (IRB) approval from a hospital. Patients can then be recruited.
Amid such innovative research at Purdue, it’s no wonder that faculty are constantly recruited by other universities and industry. Irazoqui says he sees himself nowhere else but Purdue.
“The difference between being at Purdue and being any other place is the sheer number and diversity of faculty you find here,” he says. If you want to build a team to tackle a problem, there is no place like Purdue to find engineers who are good at the 10 different things that are critical to making a system that will address the clinical need.”

Comments