Degrees & Training
Degree Programs
The Purdue College of Engineering includes three degree programs: Biomedical Engineering PhD, Combined Clinical MD/PhD BME Physician-Engineer Training Program, and the MS BME program for medical students.
Biomedical Engineering PhD
The PhD options in biomedical engineering are highly interdisciplinary in nature involving faculty at Purdue's Colleges of Engineering, Science and Veterinary Medicine on the West Lafayette campus. Doctoral program students work towards translating discoveries into effective medical products. These programs span modern biomedical engineering and build on a deep history of research that has had significant industrial and clinical impact.
MD/PHD BME Physician-Engineer Training Program (MSTP)
The field-defining collaborative Medical Scientist Training Program (MSTP) was initiated in 2008 to educate the next generation of physician-engineers through integrated MD and PhD training. It continues to garner recurring National Institutes of Health funding and significant accolades. The program sets the trends in academic medicine and industry as to how advanced technologies and approaches can optimally improve patient care and clinical outcomes. It is for students committed to a career that intimately integrates engineering design and translational research with clinical care.
There have been more than three dozen graduates of this hallmark program. These graduates are intimately involved in a burgeoning number of clinical trials at Indiana University Health to evaluate the latest advances in both hospital and clinic settings.
MS BME Program for Medical Students
A research-based master's degree program was established in 2018 in the Purdue College of Engineering for Indiana University School of Medicine medical students seeking to earn both MD and MS BME degrees. The seamless integration of the timelines for the two degrees allows these students to complete both degrees in five years.
The MS BME program for medical students leverages the students' clinical training and medical school coursework to advance innovative engineering solutions for challenges in healthcare delivery. Significant areas for translational research projects include implantable medical devices, engineered tissues and biomaterials, point-of-care diagnostics, advanced medical imaging, and systems engineering of healthcare delivery.
Students earning this degree gain firsthand knowledge of medical technology innovation and strategies for clinical translation. They will strengthen their ability to pursue medical research, to facilitate clinical testing of new therapies, and to collaborate effectively with the biomedical industry.
Auditory Neurosciences Training Group
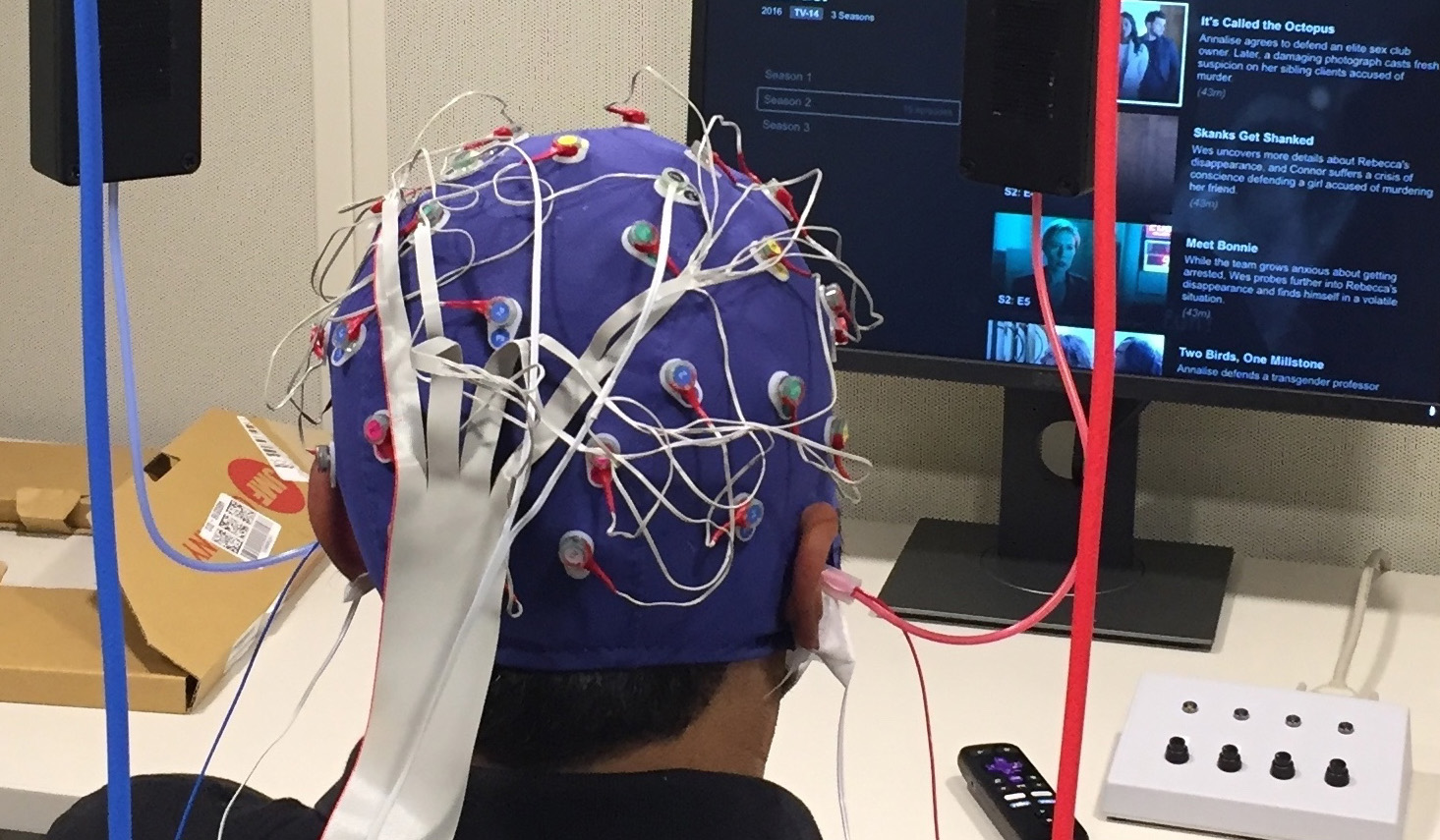
Launched in 2018, the Auditory Neurosciences Training Group (ANTG) offers a training program at the intersection of auditory neuroscience and innovation technologies, such as neuroimaging, stimulation devices, electrophysiology and mathematical modeling. The program targets a highly diverse cadre of doctoral students for translational research in speech and hearing science and technologies.
Prospective Students
Learn more on our Graduate Programs webpage.