How do you identify problems in health care that have potential technological solutions without actually being immersed in a clinical setting? On the flip side, how do you work with cutting-edge medical devices without a core understanding of the technology these devices leverage to solve critical health care challenges?
A powerful collaboration between the Purdue University Weldon School of Biomedical Engineering and Indiana University School of Medicine (IUSM) is specifically addressing these challenges. The strategic initiatives under the large umbrella of this interdisciplinary collaboration leverage the complementarity of the two world-class institutions, says George Wodicka, the Dane A. Miller Head of the Weldon School of Biomedical Engineering at Purdue, who has been one of the early molders of the multi-pronged collaboration. “At its heart is a mission of improving health care and the lives of patients while fulfilling the needs of a large number of stakeholders involved in what we do,” Wodicka says. The most important stakeholders? The students.
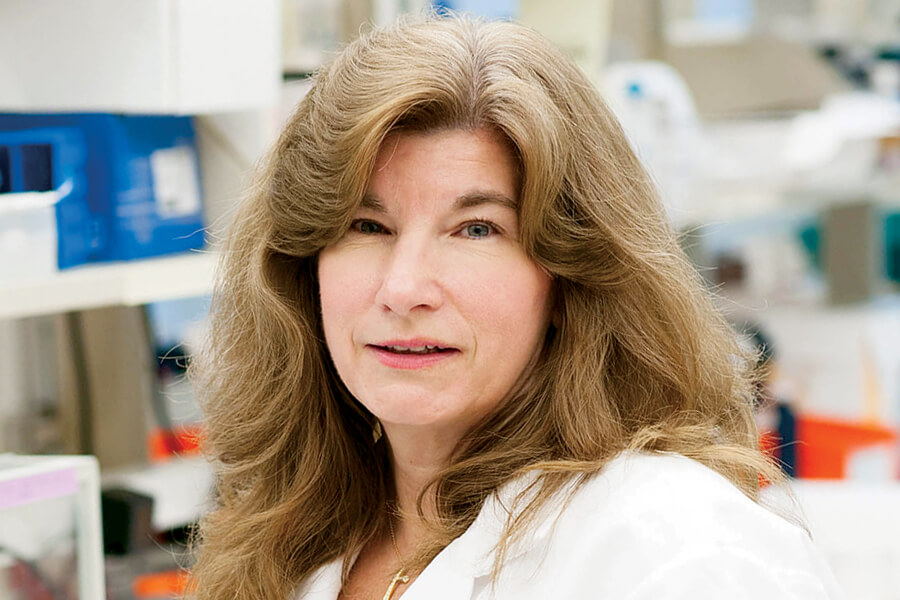
Motivated and innovative students are drawn to the dynamic exchange of expertise, which takes place through two primary channels: combined degree and specialty cross-disciplinary training program, and multidisciplinary collaborative research projects. Ongoing student-mentor engagement gives students a unique perspective, says Sherry Harbin, professor of biomedical engineering, and professor of basic medical sciences at Purdue. “Our students learn the language of clinicians, and the clinicians learn the language of engineers. They learn how folks approach things on either side, and they can really facilitate crosstalk and exchange of ideas,” Harbin says. It creates a special interface between the two disciplines, one that births innovative engineering solutions to medical needs.
Harbin is keenly aware that powerful minds with different training under their belts must navigate tricky spaces when collaborating on teams for long-term projects. “Everybody might have different approaches, different concerns, different goals, but the key is communication,” she says. “Never disrespect a position.”
Such deep-rooted synergy and robust approaches have yielded rich dividends. Students repeatedly report being especially impressed by the opportunities for collaboration and the daily communication between the two campuses in central Indiana.
The students, Wodicka notes, form the glue that holds everything together. “They bring the faculty together not only from a scientific standpoint but also from an interrelational one,” he says. “The greater the number of students we have working at this interface and bringing faculty from the School of Medicine and our College of Engineering together, the more these programs will expand their impact.”
New in 2018: A new combined MD/MS BME degree program, an Innovation for Clinical Translation (ICT) Fellowship program, and expansion of summer research opportunities for medical students in biomedical engineering are a few of the initiatives to invigorate this collaboration toward creating advanced medical technologies.
In light of the long-term success the two institutions have generated over the years and the new initiatives of 2018, the inter-institutional activities are certainly expected to grow and be even more fruitful.
Degree Programs
Integrating Health Care and Engineering
Formal collaborations between Indiana University School of Medicine (IUSM) and the Purdue University Weldon School of Biomedical Engineering have led to a flourishing combined MD/PhD physician-biomedical engineer program and the launch of a new MD/MS BME combined degree program.
MD/PhD Program
It was in the early 1960s that the National Institutes of Health decided to do something about a growing problem: physicians who lacked research training. Providing funding support for combined MD and PhD programs addressed this challenge, as it introduced medical students to the rigors of traditional research training as well as to clinical practice. While traditional MD/PhD programs are often oriented around biomedical science research, the IUSM decided to include significant training in biomedical engineering to make for a stronger and unique offering. Thus, a collaboration with the Weldon School.
Since 2002, the IUSM-Purdue MD/PhD in biomedical engineering program, offered as a partnership between the two schools, has selected and fully funded highly qualified admitted students. Roughly one-third of the 60 MD/PhD students at IUSM each year complete doctoral research training in biomedical engineering.
Dr. Raghu Mirmira is the Eli Lilly Professor in Pediatric Diabetes; director of the Herman B Wells Center for Pediatric Research; director of and co-director of the MD/PhD program, along with Maureen Harrington, associate dean for medical student education, at IUSM. He says that the medical profession is not just focused on learning how and why a disease occurs and how to prevent it, but also how to treat it with technology. This is where engineers are especially useful, he points out.
Take the case of diabetes. “You have to be able to deliver insulin at the right time and at the right dosage depending on the blood sugar levels,” Mirmira says. “It’s a mathematical and mechanical problem. If you’re an engineer, you have the tools to generate algorithms with decision processes that can determine the right dosage. Engineers develop the pumps and sensors that address this problem, and having a view from both sides leads to a more well-rounded approach.”
The training time for the IUSM-Purdue combined MD/PhD program usually clocks in at eight years, with students switching to the PhD program after two years of medical school and then returning to complete clinical training after receiving a PhD degree. Coursework overlap between the two schools shaves off close to a year of required time and credits.
MD/MS Program
The new MD/MS program in biomedical engineering, which launched in 2018, grew out of the need for a more concentrated dose of biomedical engineering over a shortened span of around a year, says George Wodicka, the Dane A. Miller Head of the Weldon School. Launching this program allows more medical students to gain exposure to biomedical technologies and participate in related research projects. “The medical students take a year off and undertake a master’s in biomedical engineering to better understand how medical devices are designed, built, tested and approved,” Wodicka says.
Essentially, the MD/MS BME program immerses medical students in an engineering setting where they learn the process of designing cutting-edge medical devices and technologies. Students can also conduct substantive research in future-forward areas from the ambulatory monitoring of chronic diseases to implantable therapeutic devices.
“These programs bring together the brightest people who are interested in optimizing their educational experiences and in reaching professional goals,” Wodicka says. “Collectively, our joint educational offerings are highly synergistic. For example, master’s students may benefit from a number of PhD students in the lab doing advanced research on a topic where they might be developing a specific application. There’s a potential for collaborative resonance, and that’s what we strive for.”
ICT Fellowship Program
The process of developing medical technologies to solve clinical and health-related problems is challenging and requires frequent iterations between the lab and the clinical setting. Clinical trials, for example, can be a complex process but a necessary part of product development. The Innovation for Clinical Translation (ICT) Fellowship Program, launched in 2018, allows PhD students in biomedical engineering to become fully immersed in a pertinent clinical environment.
The fellowship gives engineering students an opportunity for significant interactions with clinical mentors and clinical settings says Andrew Brightman, assistant head of biomedical engineering and associate professor of engineering practice at Purdue. The students have both engineering and clinical mentors to help understand how the pathways intersect. “It’s a more integrated process of having clinical ideas interfacing with engineering,” he says. “You don’t let the technology dictate direction and then go find out if it works in a patient later. You start with what is a clinical need and then as you develop the product, you work closely with health care providers, so at the end point it performs well in the clinic.”
The program is funded jointly by the Purdue College of Engineering and IUSM. The focus, says Brightman, is on students who are seeking to apply technologies in clinical practice, such as hospital and ambulatory care settings.
Under the supervision of medical faculty, these students are expected to shine light on the most pressing problems in medicine and to then execute an engineering approach to develop tools that might find ready patient adoption. “The students get to spend time in the clinical setting, have clinical mentors, and better understand clinical problems,” Brightman says. “While we have had research collaborations before, this is a much more directed, immersive program.
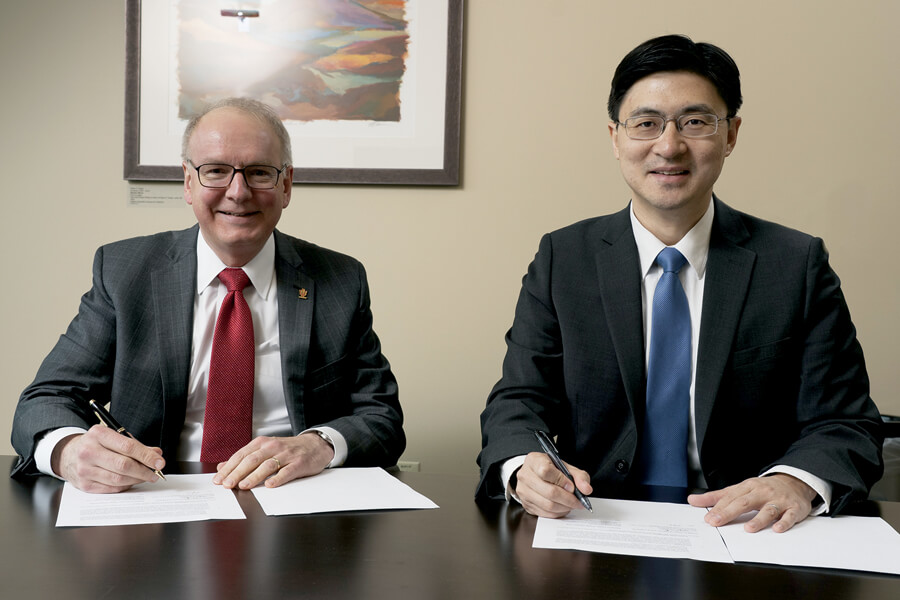
One of the significant aspects of the collaboration between the two institutions is the level of initiation and guidance from the deans, Brightman says. Indeed, the ICT Fellowship program was born from the shared visions of Mung Chiang, the John A. Edwardson Dean of the Purdue College of Engineering, and Dr. Jay L. Hess, dean of IUSM.
The more integrated process of design and development with clinical immersion is just the right prescription for an industry where technology is constantly changing. Tighter iterations between product design, development and clinical testing lead to breakthroughs in important medical diagnosis and treatment. Purdue and IUSM faculty both have high expectations for this new program, where technologists and clinicians work hand-in-hand to solve the most pressing health challenges of the day.
Strength in Numbers
The collaboration between the Purdue University Weldon School of Biomedical Engineering and Indiana University School of Medicine extends beyond academic programs and research projects.
Andrew Brightman, assistant head of biomedical engineering and associate professor of engineering practice at Purdue, points out that the ecosystem fosters continuous efforts to find areas that can leverage the strengths of both institutions and seek funding for future projects. The NIH-funded Bioengineering Interdisciplinary Training in Diabetes Research (BTDR) program, for example, was born out of the synergy between one of IUSM’s primary strengths: diabetes research and the engineering innovation strength of the Weldon School. Similarly, the Auditory Neurosciences Training Group (ANTG) is a vehicle for students and faculty to share ideas and collaborate on next-generation approaches for speech and hearing science technologies.
“We continuously bring key individuals from the two institutions together to brainstorm about potential new projects and eventually write grant proposals together,” Brightman says.
George Wodicka, the Dane A. Miller Head of the Weldon School of Biomedical Engineering, says the NIH T32 training grants have proven to be fertile ground for the best minds at the two institutions to come together. “Once we obtain training grants following integrated themes and approaches, we use them as seeds to accelerate the research process through dedicated courses and a broader exchange of ideas,” Wodicka says.
Students also enjoy the advantage of advising from both institutions as faculty members from the two schools mentor graduate students on research direction and goals. “It really is an amazing time to be in biomedical engineering,” Wodicka says. “Our students leverage our world-class collaboration, and they lead the charge. I’m confident that many future technological advances in health care will stem from these cross-trained students for decades to come.”
Research Projects
Indiana University School of Medicine (IUSM) and the Purdue University Weldon School of Biomedical Engineering continue to collaborate on a variety of research projects across a variety of specialties.
Here are two promising examples that are on the road to commercial market maturity:
What: A Less Intrusive Way to Manage Type 1 Diabetes
The Problem: Managing Type 1 diabetes involves daily insulin injections or having to wear a pump.
How Addressed: Collagen protein piggybacking on pancreatic cells, delivered through a shot, is found to reverse Type 1 diabetes and maintain dependence on insulin for at least 90 days.
Who: Weldon School of Biomedical Engineering researchers Sherry Harbin, professor of biomedical engineering and basic medical sciences, and Clarissa Hernandez Stephens, graduate researcher and Innovation for Clinical Translation (ICT) Fellow. Dr. Raghu Mirmira, Eli Lilly Professor in Pediatric Diabetes and director of the Center for Diabetes Research and Metabolic Diseases at IUSM.
What’s Next: Purdue’s College of Veterinary Medicine will be the staging ground for a pilot clinical study of this treatment approach in dogs with naturally occurring Type 1 diabetes.
What: Super-Resolution “Nanoscope” for Advanced Brain Imaging
The Problem: Single molecule super-resolution imaging in brain tissues poses significant challenges. The sample-induced aberrations distort and blur single-molecule emission patterns.
How Addressed: The use of “deformable” mirrors allows detecting and pinpointing single fluorescent molecules with nanometer precision and reconstructing fine details of fibrillar amyloid-β plaques found in Alzheimer’s disease in 30 μm brain sections.
Who: Gary Landreth, professor of anatomy and cell biology at IUSM’s Stark Neurosciences Research Institute, and Fang Huang, assistant professor of biomedical engineering in the Weldon School.
What’s Next: Further exploration of how amyloid plaques affect and damage other brain cell types during the progression of Alzheimer’s disease.


